Did you know that over 58 million Americans report living with arthritis? [1]
Joint pain, whether from a disease or another cause, is a widespread problem that can strike at any age, and in any joint.
Hands, knees, feet, hips, ankles, and shoulders are commonly affected.
Whether you've experienced joint pain for the first time, or have been struggling with ongoing discomfort, this article is your friend.
We'll explore:
- Why your joints hurt
- Warning signs you shouldn't ignore
- 6 relief strategies that actually help
By the end, you'll have the information to take the next step towards addressing the issue and improving your joint comfort.
Key Takeaways
- Joint pain can be the result of overuse, injury, or arthritis, but not every ache is a serious condition.
- Red flags include pain that doesn't go away, swelling, heat, stiffness, or fever; in these cases, it's best to see a doctor.
- Arthritis comes in different forms, including osteoarthritis, rheumatoid arthritis, and gout. [2]
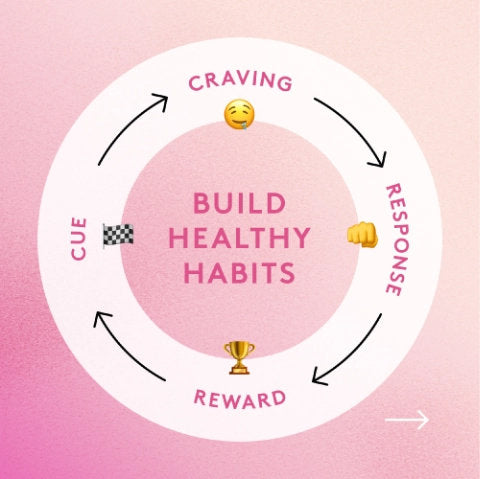
- Other factors that can worsen joint pain include physical inactivity, nutrient gaps, poor diet, or lack of sleep. [3, 4, 5]
- Daily low-impact exercise (30-60 minutes) can strengthen joints.
- Anti-inflammatory, prebiotic-rich foods and targeted support (e.g., our Performance Lab® Flex) can promote joint comfort.
Why Joints Hurt: Wear-and-Tear, Deficiencies, and Common Causes of Joint Pain

The frustrating part about joint pain is pinpointing where it comes from. Especially if you've lived healthily and without issues before pain crept in.
The good news is, figuring out the cause is already a big first step to resolving the issue. When we know the culprit, we know what to target.
So, here is the list of most common causes of painful joints:
- Arthritis types - this includes osteoarthritis, rheumatoid arthritis, gout, and many other types of arthritis and related conditions. The hallmark of arthritis is chronic, ongoing inflammation and breakdown of joint tissues, which sometimes shows up as pain, swelling, or stiffness (or all three together). [6]
- Injuries - sprains, strains, tears, or fractures of joint structures can cause aches, discomfort, and other unexplained symptoms.
- Overuse - common in athletes, computer users, and certain manual jobs, overuse of joints through repetitive motion can lead to inflammation or an injury, resulting in pain or conditions like tendonitis. [7]
- Autoimmune triggers - When the body mistakes its own tissues as invaders, it attacks them, which can lead to autoimmune reactions such as pain, swelling, and inflammation in joints. This is what happens in rheumatoid arthritis. [8]
Also consider lifestyle factors like:
- Sedentary habits that weaken joint-supporting muscles
- Nutrient deficiencies like vitamin D, calcium, and magnesium [9]
- Poor sleep aggravating inflammation levels [10]
- Diet loaded with ultraprocessed foods that promote systemic inflammation and joint pain [11]
While the above lifestyle habits may not necessarily cause joint pain, they can still play their part in making joint pain worse.
When Joint Pain Deserves Your Attention

Joint pain isn't always a reason for alarm.
That said, warning signs include swelling, tenderness, warmth, pain, redness, fever, or loss of movement.
If you have pain in multiple joints, it can signal a systemic issue like an autoimmune flare. [12]
While not extremely common, joint infections and bone infections can also cause pain; these should be addressed immediately. [13]
If your symptoms include warmth, tenderness, redness, or pain, call a doctor.
Conditions That Show Up First as Painful Joints (Arthritis Pain, Gout, and More)
Painful joints can sometimes be the first sign of a deeper problem.
Common types of arthritis, like osteoarthritis, RA, and gout, often show up first as joint pain, along with other symptoms like joints stiff, swelling, reduced mobility, or even fatigue. [2]
The main types include:
- Osteoarthritis - a degenerative joint disease caused by wear and tear of the cartilage in joints.
- Rheumatoid arthritis (RA) - an autoimmune disease where the immune system mistakenly attacks joint tissues.
- Gout - an inflammatory arthritis known for sharp, sudden pain, often in the big toe, triggered by uric acid crystal buildup in joint tissues. [2]
Other conditions that can begin with joint pain include:
- Lupus - an autoimmune disease where the body attacks its own healthy tissue (not just joints), felt as fatigue, fever, joint pain, and rashes, and sometimes mixed up with rheumatoid arthritis. [14]
- Psoriatic arthritis - an inflammatory condition that triggers joint pain, skin rashes, and nail changes. [15]
Less common links include multiple sclerosis (MS) and diabetes, where nerve damage and inflammation can lead to pain. [16, 17]
6 Study-Backed Ways to Ease Joint Pain

-
Low-Impact Exercise for Joint Stability and Relief
Exercise is essential for maintaining muscle mass. Strong muscles help stabilize joints, take off the pressure, and improve flexibility.
Regular exercise may also lower inflammation markers linked to joint pain. [18]
Choose moderate-intensity exercise that doesn't put pressure on joints (think swimming, cycling, or power walking). Avoid running.
Moderate effort, where you can talk but not sing, is ideal, but even lighter activity helps. Aim for 30-60 minutes of training per day.
Weightlifting (strength training) is also shown to promote joint comfort and long-term resilience. [19] Start slow and increase intensity over time. If you feel pain during exercise, stop and try another movement instead.
-
Anti-Inflammatory Diet to Ease Pain and Swelling
You'll often see Mediterranean-style diet as a nutrition recommendation for relieving joint pain and other symptoms like stiffness and swelling. Studies show it may indeed help. [20]
This diet focuses on fruits, vegetables, whole grains, olive oil, nuts, seeds, and fatty fish. It avoids ultra-processed foods, refined sugar, and excessive amounts of saturated fat.
Prebiotics in these foods feed healthy gut bacteria, which help regulate inflammatory processes and may ease joint pain. [21]
-
Rest, Ice, Compression, Elevation (RICE) for Short-Term Injury Relief
RICE is a common method of soothing minor injuries and joint pain. It's often applied to the affected joint within 24-48 hours after an injury.
However, there is surprisingly a lack of strong evidence to prove effectiveness compared to other treatments. [22]
-
Physiotherapy for Long-Term Joint Health
A physical therapist can develop a plan for your specific case; whether that's a joint injury or a chronic problem. This can help if other methods didn't relieve pain.
A therapist may use techniques like hot and cold therapy, deep tissue massage, laser therapy, shockwave therapy, and specialized exercise programs.
-
OTC Anti-Inflammatories for Occasional Pain Relief
OTC pharmaceuticals, such as non-steroidal anti-inflammatory drugs or topical medications, can reduce mild or moderate joint aches. [23]
But since these drugs mask pain, it's easy to overuse the joint and add to the problem.
Due to a long list of possible side effects, it's best not to rely on them long-term.
-
Targeted Supplements for Inflammation and Cartilage Support
Certain nutrients and herbs may soothe inflammation and joint discomfort.
These include omega-3 fatty acids, curcumin+ black pepper, MSM, Boswellia Serrata, and collagen peptides. [24]
Together, these ingredients may support joint comfort and cartilage health, though results vary.
Performance Lab® Flex combines well-studied ingredients like CurcuWIN® turmeric and AprèsFlex® Boswellia Serrata for targeted joint support.
On the other hand, Performance Lab® Omega-3 is a clean, algae-based omega-3 supplement for anyone looking to ease joint inflammation.
Combine Flex with Omega-3 for comprehensive support.
Pain on Joint – By Location

Fingers
Finger joint pain (including index and middle finger) can come from injuries, repetitive use, or autoimmune diseases like arthritis.
Finger pain that fades on its own is usually not a reason for concern. However, early warning signs of stage 1 rheumatoid arthritis can include pain in finger joints along with swelling, deformity, and heat sensations. [25]
In this case, your relief strategies include splints, heat therapy, and activity modification.
Thumb
Much like with other fingers, thumb pain can be caused by thumb arthritis (basal joint arthritis), repetitive strain, or injury. Early signs include pain at the base and reduced grip strength. [26]
Can thumb arthritis resolve on its own? In most cases, no. While symptoms may improve with rest, the underlying disease still needs to be addressed.
If you have thumb pain, it's possible to get relief through:
- Hand therapy
- Steroid injections
- Medications (for occasional flare-ups or short-term management)
- Splinting
- Stretches
- Supplements targeting inflammation and joint pain
Knee (Pain on Joint Line of Knee)
If you're dealing with knee pain, you're not alone. An estimated 1 in 4 adults experience it. [27]
Most common causes include meniscus tears, osteoarthritis (OA), and ligament injuries.
Joint line tenderness is a common test for meniscus injury or arthritis. [28] It involves pressing on joint surfaces or moving the joint through its normal range of motion to check sensitivity.
If you have knee pain red flags, which include severe pain, difficulty bearing weight, swelling, fever, or inability to move the knee, get a professional evaluation as soon as possible.
Sudden, sharp pain suggests an injury. If it’s more dull or achy and comes with stiffness and swelling, then it should be checked for arthritis, which often affects the knee along with other joints.
Feet
Pain on joints of feet is quite common. Our feet are daily shock absorbers.
And while feet are designed for daily activity, nagging pain may point to arthritis, plantar fasciitis, injury, or overuse (or a combination of these).
While feet injuries can heal, rheumatoid arthritis is notorious for getting worse over time. [25] In early stages of arthritis, symptoms might not be obvious, and the condition can't be easily diagnosed.
Tell-tale signs of foot arthritis include swelling and stiffness.
Foot pain can also happen during pregnancy due to weight gain and hormonal changes. [29]
Treatment options for foot pain depend on the cause, but typically include physical therapy, footwear changes, dietary modifications, and supplements for joint support.
Big Toe
Big toe pain affects ball of the foot, at the joint base.
It can be caused by gout, a form of arthritis where uric acid crystals buildup in the toe, causing sharp joint pain. [30]
If the pain is more gradual, it could involve sesamoiditis, an inflammatory condition caused by a strain or injury to the sesamoid bone and surrounding tissues around the ball of the foot. [31]
Other potential causes of big toe pain include fractures, and other forms of arthritis such as hallux rigidus, which causes pain, stiffness, and difficulty walking. [32]
Depending on the cause, your relief strategies include targeted footwear, anti-inflammatory nutrition, professional therapy, and joint supplements.
Multiple Joints Hurting? Here's What It Could Mean

If you have unexplained joint pain in different areas, it could mean an immune system problem, gout, or another joint disorder, and is a clear sign to get checked by a specialist.
Here's the kicker, though: your gut health plays a key role in joint inflammation and pain.
It houses trillions of bacteria that can drive or calm inflammation. Moreover, research suggests the gut microbiome may play an important role in arthritis. [21]
- A 2015 study led by dr. Jose Scher found a link between psoriatic arthritis and decreased gut microbe diversity. [33]
- A recent 2022 review supports these findings; suggesting that gut microbiota imbalances can disrupt immune tolerance and contribute to rheumatoid arthritis. [34]
So, what are some practical takeaways? Avoid ultraprocessed foods, fried oils, and refined sugar. Just as importantly, sleep well, manage stress, quit smoking, and stay active. All of these influence gut and joint health.
Your Next Moves for Stronger, Healthier Joints (Joint Pain Relief That Lasts)

Your first step is to identify and address the culprits of joint pain. Whether it's injury, arthritis, overuse, or something else.
Watch for red flags like sudden or sharp pain, swelling, heat, or pain in multiple joints. These are all signals to seek professional opinion.
Support your joints daily with low-impact exercise that you can handle, and a nutrient-diverse meal plan focused on gut-friendly, anti-inflammatory foods.
Performance Lab Flex for Daily Joint Comfort

For additional joint support, take Performance Lab® Flex: a multi-ingredient formula made to promote pain-free movement and daily comfort. It won't replace good habits, and results can vary, but its gentle ingredient profile is ideal for anyone looking for a safe, high-quality, daily joint supplement.
Be proactive. Small, consistent steps now can ease joint pain and protect mobility in the long run.
References
- Eze, B., Green, J. T., Asante, R., Okobi, O. E., Mercene, K. G. F., Ogbodo, C. T., Anamazobi, E. G., & Alozie, A. S. (2024). Trends in Arthritis Prevalence and Associated Chronic Health Indicators Among Adults: Insights From the Behavioral Risk Factor Surveillance System (BRFSS) Database. Cureus, 16(4), e58925. https://doi.org/10.7759/cureus.58925
- Senthelal S, Li J, Ardeshirzadeh S, et al. Arthritis. [Updated 2023 Jun 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK518992/
- Lee, S.-H., Son, C., Yeo, S., & Ha, I. H. (2019). Cross-sectional analysis of self-reported sedentary behaviors and chronic knee pain among South Korean adults over 50 years of age in KNHANES 2013–2015. BMC Public Health, 19, Article 1375. https://doi.org/10.1186/s12889-019-7653-9
- Sibille, K. T., King, C., Garrett, T. J., Glover, T. L., Zhang, H., Chen, H., Reddy, D., Goodin, B. R., Sotolongo, A., Petrov, M. E., Cruz-Almeida, Y., Herbert, M., Bartley, E. J., Edberg, J. C., Staud, R., Redden, D. T., Bradley, L. A., & Fillingim, R. B. (2018). Omega-6: Omega-3 PUFA Ratio, Pain, Functioning, and Distress in Adults With Knee Pain. The Clinical journal of pain, 34(2), 182–189. https://doi.org/10.1097/AJP.0000000000000517
- Afolalu, E. F., Ramlee, F., & Tang, N. K. Y. (2018). Effects of sleep changes on pain-related health outcomes in the general population: A systematic review of longitudinal studies with exploratory meta-analysis. Sleep medicine reviews, 39, 82–97. https://doi.org/10.1016/j.smrv.2017.08.001
- Smolen, J. S., Aletaha, D., & McInnes, I. B. (2016). Rheumatoid arthritis. The Lancet, 388(10055), 2023–2038. https://doi.org/10.1016/S0140-6736(16)30173-8
- Kaux, J. F., Forthomme, B., Goff, C. L., Crielaard, J. M., & Croisier, J. L. (2011). Current opinions on tendinopathy. Journal of sports science & medicine, 10(2), 238–253. https://pmc.ncbi.nlm.nih.gov/articles/PMC3761855/
- Alivernini, S., Firestein, G. S., & McInnes, I. B. (2022). The pathogenesis of rheumatoid arthritis. Immunity, 55(11), 2255–2270. https://doi.org/10.1016/j.immuni.2022.11.009
- Montemor, C. N., et al. (2025). Impact of Reduced Vitamin D Levels on Pain, Function, and Inflammatory Biomarkers in Hip and Knee Osteoarthritis. Nutrients, 17(3), Article 447. https://doi.org/10.3390/nu17030447
- Irwin, M. R., Olmstead, R., Carrillo, C., Sadeghi, N., Fitzgerald, J. D., Ranganath, V. K., & Nicassio, P. M. (2012). Sleep loss exacerbates fatigue, depression, and pain in rheumatoid arthritis. Sleep, 35(4), 537–543. https://doi.org/10.5665/sleep.1742
- Tristan Asensi, M., Napoletano, A., Sofi, F., & Dinu, M. (2023). Low-Grade Inflammation and Ultra-Processed Foods Consumption: A Review. Nutrients, 15(6), 1546. https://doi.org/10.3390/nu15061546
- Chauhan, K., Jandu, J. S., & Brent, L. H. (2025). Rheumatoid arthritis. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441999/
- Colston, J., & Atkins, B. (2018). Bone and joint infection. Clinical medicine (London, England), 18(2), 150–154. https://doi.org/10.7861/clinmedicine.18-2-150
- Justiz Vaillant, A. A., Goyal, A., & Varacallo, M. A. (2025). Systemic lupus erythematosus. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK535405/
- Azuaga, A. B., Ramírez, J., & Cañete, J. D. (2023). Psoriatic Arthritis: Pathogenesis and Targeted Therapies. International journal of molecular sciences, 24(5), 4901. https://doi.org/10.3390/ijms24054901
- ShayestehAzar, M., Kariminasab, M. H., Saravi, M. S., Abedini, M., Fazli, M., Hashemi, S. A., & Abdizadeh, P. (2015). A Survey of Severity and Distribution of Musculoskeletal Pain in Multiple Sclerosis Patients; a Cross-Sectional Study. The archives of bone and joint surgery, 3(2), 114–118. https://pmc.ncbi.nlm.nih.gov/articles/PMC4468621/
- Eitner, A., & Wildemann, B. (2021). Diabetes - osteoarthritis and joint pain. Bone & joint research, 10(5), 307–309. https://pmc.ncbi.nlm.nih.gov/articles/PMC8160031/
- Kong, H., Wang, X. Q., & Zhang, X. A. (2022). Exercise for Osteoarthritis: A Literature Review of Pathology and Mechanism. Frontiers in aging neuroscience, 14, 854026. https://pmc.ncbi.nlm.nih.gov/articles/PMC9110817/
- Harvard Health Publishing. (2024, February 1). Strength training tied to smaller risk of knee osteoarthritis and pain later in life. Harvard Health. Retrieved from https://www.health.harvard.edu/diseases-and-conditions/strength-training-tied-to-smaller-risk-of-knee-osteoarthritis-and-pain-later-in-life
- Veronese, N., Ragusa, F. S., Dominguez, L. J., Cusumano, C., & Barbagallo, M. (2024). Mediterranean diet and osteoarthritis: an update. Aging clinical and experimental research, 36(1), 231. https://link.springer.com/article/10.1007/s40520-024-02883-8
- Aziz, T., Hussain, N., Hameed, Z., & Lin, L. (2024). Elucidating the role of diet in maintaining gut health to reduce the risk of obesity, cardiovascular and other age-related inflammatory diseases: recent challenges and future recommendations. Gut microbes, 16(1), 2297864. https://doi.org/10.1080/19490976.2023.2297864
- van den Bekerom, M. P., Struijs, P. A., Blankevoort, L., Welling, L., van Dijk, C. N., & Kerkhoffs, G. M. (2012). What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults?. Journal of athletic training, 47(4), 435–443. https://doi.org/10.4085/1062-6050-47.4.14
- Magni, A., Agostoni, P., Bonezzi, C., Massazza, G., Menè, P., Savarino, V., & Fornasari, D. (2021). Management of Osteoarthritis: Expert Opinion on NSAIDs. Pain and therapy, 10(2), 783–808. https://pmc.ncbi.nlm.nih.gov/articles/PMC8586433/
- Liu, X., Machado, G. C., Eyles, J. P., Ravi, V., & Hunter, D. J. (2018). Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. British journal of sports medicine, 52(3), 167–175. https://doi.org/10.1136/bjsports-2016-097333
- Chauhan, K., Jandu, J. S., & Brent, L. H. (2025). Rheumatoid arthritis. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441999/
- Dias, R., Chandrasenan, J., Rajaratnam, V., & Burke, F. D. (2007). Basal thumb arthritis. Postgraduate medical journal, 83(975), 40–43. https://doi.org/10.1136/pgmj.2006.046300
- Nguyen, U. S., Zhang, Y., Zhu, Y., Niu, J., Zhang, B., & Felson, D. T. (2011). Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Annals of internal medicine, 155(11), 725–732. https://doi.org/10.7326/0003-4819-155-11-201112060-00004
- Gupta, Y., Mahara, D., & Lamichhane, A. (2016). McMurray's Test and Joint Line Tenderness for Medial Meniscus Tear: Are They Accurate?. Ethiopian journal of health sciences, 26(6), 567–572. https://pmc.ncbi.nlm.nih.gov/articles/PMC5389077/
- Segal, N. A., Boyer, E. R., Teran-Yengle, P., Glass, N. A., Hillstrom, H. J., & Yack, H. J. (2013). Pregnancy leads to lasting changes in foot structure. American journal of physical medicine & rehabilitation, 92(3), 232–240. https://doi.org/10.1097/PHM.0b013e31827443a9
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2023, December). Gout: Overview of symptoms, causes, & risk factors. U.S. Department of Health and Human Services. Retrieved August 22, 2025, from https://www.niams.nih.gov/health-topics/gout
- Kaur, P., Carroll, M. R., & Stewart, S. (2023). The assessment and management of sesamoiditis: a focus group study of podiatrists in Aotearoa New Zealand. Journal of foot and ankle research, 16(1), 29. https://doi.org/10.1186/s13047-023-00628-w
- Tedeschi R. (2024). Case study: Gait assessment of a patient with hallux rigidus before and after plantar modification. International journal of surgery case reports, 114, 109197. https://doi.org/10.1016/j.ijscr.2023.109197
- Scher, J. U., Ubeda, C., Artacho, A., Attur, M., Isaac, S., Reddy, S. M., Marmon, S., Neimann, A., Brusca, S., Patel, T., Manasson, J., Pamer, E. G., Littman, D. R., & Abramson, S. B. (2015). Decreased bacterial diversity characterizes the altered gut microbiota in patients with psoriatic arthritis, resembling dysbiosis in inflammatory bowel disease. Arthritis & rheumatology (Hoboken, N.J.), 67(1), 128–139. https://doi.org/10.1002/art.38892