We’ve always looked at the immune system and the gut as two separate entities; the gut helps us digest our food and provides us with the nutrients we need to function, whereas the immune system keeps us protected from external and internal threats.
But after decades of research, the line between these two systems is blurry. It’s not a matter of bacteria staying on one side of the line, and we remain on the other.
As it turns out, the immune system and the gut are intricately connected, and the relationship between them isn’t as simple as you may think.
A huge portion of the immune system is actually in the gut, which means keeping one healthy means keeping the other healthy. So, if you’re new to the bidirectional relationship between gut health and the immune system, you’re in for a treat.
We’re going to enlighten you on how these two systems are connected and why good gut health is imperative for a healthy immune system.
Key Takeaways
- Roughly 70% of the immune system is associated with the gut, making digestive health central to immune resilience.
- A balanced microbiome and strong gut barrier help your body distinguish friends from foes, reducing chronic inflammation and autoimmunity risk.
- Dysbiosis — an imbalance of gut bacteria — has been linked to conditions like IBD, obesity, allergies, and metabolic and autoimmune diseases.
- Stress, poor diet, lack of fiber, alcohol, and certain medications can disrupt gut health and, in turn, immune function.
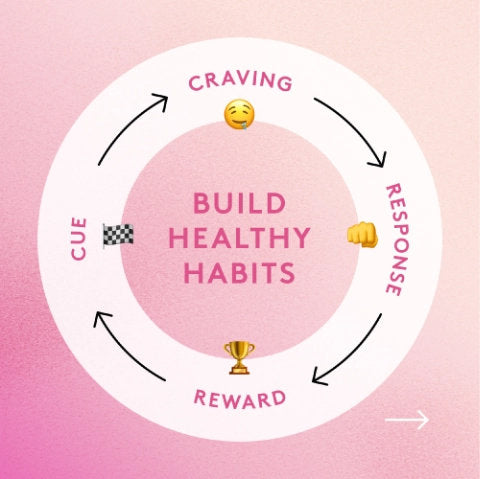
- Supporting the gut with fiber-rich foods, fermented foods, pre- and probiotics, stress management, and smart supplementation helps keep immune defenses on track.

What Is Gut Health And Why Is It Important?
When most of us think about the gut, digestion often springs to mind. Our gut is responsible for keeping our body working; it breaks down the food we eat and absorbs nutrients to support proper body functions.
Whether that’s energy production and hormonal balance, or mental health and toxin removal, the gut has many important jobs that make keeping it healthy a huge deal.
But when things go sideways and the gut isn’t such a healthy place, you start to develop imbalances between the good and bad bacteria that inhabit it.
Under normal healthy conditions, the good guys keep the bad guys in check; they should outnumber them, which maintains homeostasis (balance).
However, when stress gets out of hand, we’re not eating properly, over-exercising, consuming a few too many drinks, or aren’t sleeping enough, the bad guys can outnumber the good, and we’re left with a state of imbalance, more technically known as dysbiosis.
A healthy intestinal microbial environment is characterized by the diversity, stability, resistance, and resilience of the ecosystem.
Several factors can affect the balance of the environment, which results in compositional and functional alterations in the microbiota 1. This is termed dysbiosis. And once this microbial balance is shifted, dysbiosis will persist until the balance is reestablished.
In normal, healthy conditions, there is major crosstalk and cross-regulation between the host (the person) and the microbes that reside in the gut, which creates a homeostatic balance of bacteria to ensure the gut remains healthy and prevents pathogenic bacteria from proliferating.
The microbiota offers a mutually beneficial relationship; the bacteria thrive in the rich environment of the gut, while the person benefits from a host of functions offered by the bacteria 2.
The reason we talk about dysbiosis is because microbial imbalances in the gut are basically a breeding ground for disease.
Because the health of the gut has such far-reaching impacts on the health of every other system in the body, dysbiosis has been implicated in several diseases, including 2:
- Inflammatory bowel disease (Crohn’s, ulcerative colitis)
- Obesity
- Allergies
- Type 1 diabetes mellitus
- Autism
- Colorectal cancer
- Autoimmunity
- Chronic inflammation
The Link Between Gut Health And The Immune System
Contrary to what most people think about the gut, it’s not just for supporting digestion and nutrient absorption. It also plays a massive role in immune function.
Over the last couple of decades, it’s become obvious that alterations of the gut microbial environment can cause immune dysregulation, leading to a host of health complications.
The GI system is the main point of contact with the external environment—the GI tract is actually open to the outside via the mouth—and is bombarded daily with stimuli, some of which are dangerous pathogens or toxic substances. This important position of the GI system is evident through many immune cells that call it home.
Gut-associated lymphoid tissue (GALT) is the largest portion of mucosal-associated lymphoid tissue (MALT), representing nearly 70% of the entire immune system 3.
And if that wasn’t enough, about 80% of plasma cells, primarily IgA-bearing cells, reside in GALT. You can think of GALT as the intestinal frontier of the systemic immune response.
GALT organs are the sites where antigens are presented to antigen-presenting cells that decide whether the inflammatory cascade happens or the body can tolerate it.
The surface of the intestine houses a thin layer of cells called epithelial cells (IECs) that separates the gut lumen from the mucosal immune system 4. Despite acting as a barrier, it plays a transport role in providing information about the external environment.
GALT is also composed of Peyer’s patches (PP), which are highly specialized gut lymphoid follicles in the wall of the small intestine that house naïve B cells, follicular dendritic cells (FDCs), and T cells.
Peyer’s patches are covered by follicle-associated epithelium (FAE) that contain specialized epithelial cells, called M cells. These M cells introduce luminal antigens to the enteric immune system to help with the development of tolerance.
In simple terms, GALT is the intersection of the GI system, the immune system, and the nervous system and comprises a network of immune cells and membranes that line the internal passages of our body.
It’s kind of like an “inside skin” that has the sole responsibility of protecting the body against external factors that penetrate the luminal mechanical barrier.
The skin functions to absorb nutrients and provide a barrier that protects toxins from entering the body. The GALT works in the same way, but internally.
But where good gut health comes into the picture is that when your gut is healthy and microbiota are balanced and thriving, these powerhouse cells of the immune system spring into action when pathogenic organisms are detected to quickly neutralize them and prevent a problem.
However, if you’re dealing with dysbiosis—an imbalance between good and bad gut flora—the immune cells present in GALT start reacting to food particles, for example, instead of the pathogenic organisms. As a result, your immune system becomes hypersensitive, and you run this risk of developing chronic gut inflammation 5.
Apart from preventing infections and curb hypersensitivity, GALT is also positively affected by the probiotic microbes that live in the gut. Studies have shown that proper GALT development in early life largely depends on its interaction with certain probiotic species, including B. fragilis and B. subtilis 6.
There’s also evidence that other probiotic strains like Lactobacillus GG, Bifidobacterium lactis, and Saccharomyces boulardii can enhance the production of IgA, a powerful antibody that binds to pathogens in the gut and marks them for destruction by other immune cells 7.
Long story short, the gut needs to be a healthy place to prevent inflammation and an overactive immune system that can result in autoimmunity.
Studies show that Bifidobacteria and Lactobacillus species induce expression of anti-inflammatory cytokines, including TGFβ and IL-102, that signal to T-regulatory cells to calm the immune system down, thus acting as damage control.
The link between the immune system and gut health is by no means straightforward. Still, the takeaway message here is that you can’t have a healthy immune system without having a healthy gut, so taking the necessary steps to get your gut balanced is critical to supporting healthy immune responses.
And how do you do that? In the next section, you'll find out!
4 Tips For Improving Gut Health
1. Manage Your Stress
Stress is a huge impediment to both the health of the gut and the function of the immune system. Chronic mismanaged stress can weaken the intestinal barrier, as well as change the composition of the microbiome via stress hormones, inflammation, and autonomic alterations.
In turn, gut bacteria release metabolites, toxins, and neurohormones that can alter eating behaviors and trigger mood imbalances 8.
If you’re feeling extra stressed, try these:
- Exercise
- Get outside
- Expose yourself to sunlight
- Do some deep breathing
- Meditate
- Journal
- Talk to a friend
- Do a brain dump before bed
2. Cut Out Sugar And Refined Carbohydrates
Diet plays a major role in the gut's health, and studies suggest that certain components of the diet can reshape gut microbiota populations and can transform a healthy gut into a diseased one 9.
The typical “Western” diet high in sugar, refined carbohydrates, and bad fats is a leading contributor of dysbiosis, which affects both host GI metabolism and immune homeostasis.
If you want to avoid this, cut back on the sugars (natural or non) and limit refined carbohydrates like white bread, pasta, pastries, ready-made meals, and the like, and instead load up on fresh fruits and vegetables, complex carbohydrates, high-quality proteins, and healthy fats.
3. Eat More Fiber
We’ve always thought about fiber for supporting bowel regularity, but it’s more. Because dietary fiber cannot be digested by human digestive enzymes, it passes through the GI tract intact. In there, it is acted on by gut microbes to produced various metabolites, including short-chain fatty acids (SCFAs).
The SCFAs are mainly acetate, propionate, and butyrate, and research has shown them to have key roles in regulating host metabolism. SCFAs are transported into systemic circulation and may elicit beneficial effects on insulin sensitivity, weight regulation, inflammation, and lipid metabolism 10.
Additionally, SCFAs act as an important energy source for the intestinal epithelial cells (especially in the colon) and contribute to the strengthening of the gut barrier 11, 12. Better gut barrier integrity reduces the ability of microbes to penetrate into the bloodstream, thereby reducing immune responses.
4. Add In Probiotics + Prebiotics
Prebiotics and probiotics are all the rage when it comes to gut health. They’re incredibly powerful for repopulating the gut with beneficial bacterial species and supporting their growth and proliferation.
But while probiotics have always been the top recommendation for reducing dysbiosis, prebiotics deserve some of the spotlight. Without prebiotic fiber, the beneficial bacteria in the gut cannot survive; it’s the food that supports their growth.
While probiotic supplements are great, one of the major concerns is that they’re fragile, which means they could be dead before even making it to your gut, failing to help your microbiome in any way.
Performance Lab Prebiotic is a new kind of gut supplement that overrides all the traditional concerns around probiotics.

Instead of adding new strains of bacteria into an already stressed gut, Prebiotic focuses on nourishing the colonies that already exist in your gut using Orafti® Synergy1 (Inulin-FOS from chicory root) for robust growth and health.
It’s 2-in-1 probiotic + soluble fiber support for healthy metabolic and microbiome performance delivering safer, more natural, and more reliable microbiome support.
Final Thoughts
There’s no denying that the gut and the immune system are intricately connected, which means supporting the health of one is critical to supporting the health of the other.
And if you want to do both, there’s no better way than eating well, moving regularly, sleeping enough, and supporting both with a solid prebiotic supplement.
References
- M Levy, AA Kolodziejczyk, CA Thaiss, E Elinav. Dysbiosis and the immune system.Nat Rev Immunol. 2017;17(4):219-232.
- AK DeGruttola, D Low, A Mizoguchi, E Current Understanding of Dysbiosis in Disease in Human and Animal Models.Inflamm Bowel Dis. 2016;22(5):1137-1150.
- G Vighi, F Marcucci, L Sensi, G Di Cara, F Allergy and the gastrointestinal system. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):3-6.
- TW Spahn, T Modulating the intestinal immune system: the role of lymphotoxin and GALT organs. Gut. 2004;53(3):456-465.
- I Koboziev, F Karlsson, MB Grisham. Gut-associated lymphoid tissue, T cell trafficking, and chronic intestinal inflammation. Ann N Y Acad Sci. 2010;1207 Suppl 1(Suppl 1):E86-E93.
- HM Wexler. Bacteroides: the good, the bad, and the nitty-gritty.Clin Microbiol Rev. 2007;20(4):593-621.
- AN Vlasova, S Kandasamy, KS Chattha, G Rajashekara, LJ Saif. Comparison of probiotic lactobacilli and bifidobacteria effects, immune responses and rotavirus vaccines and infection in different host species.Vet Immunol Immunopathol. 2016;172:72-84.
- A Madison, JK Kiecolt-Glaser. Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition.Curr Opin Behav Sci. 2019;28:105-110.
- K Brown, D DeCoffe, E Molcan, DL Gibson. Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease (published correction appears in Nutrients. 2012 Oct;4(11)1552-3). Nutrients. 2012;4(8):1095-1119.
- MCW Myhrstad, H Tunsjø, C Charnock, VH Telle-Hansen. Dietary Fiber, Gut Microbiota, and Metabolic Regulation-Current Status in Human Randomized Trials. 2020;12(3):859.
- K Makki, EC Deehan, J Walter, F Bä The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease.Cell Host Microbe. 2018;23(6):705-715.
- KE Bach Knudsen, HN Lærke, MS Hedemann, et al. Impact of Diet-Modulated Butyrate Production on Intestinal Barrier Function and Inflammation. Nutrients. 2018;10(10):1499.