Painful joints stopping you from enjoying daily life? Stick with us.
From heat and ice to targeted supplements, here are 6 science-backed strategies for sore joint relief; whether you deal with occasional soreness or ongoing pain.
Key Takeaways
- Joints may get sore from injuries, overuse, or arthritis. Unlike muscle soreness, the discomfort can linger.
- Relief basics: heat + ice, short rest, OTC anti-inflammatories (occasional use), sleep, and an anti-inflammatory diet.
- Smart supplements may help: Boswellia, collagen, MSM, curcumin + black pepper. Plus nutrients like vitamin D, magnesium, and omega-3s.
- Movement matters. Too little weakens joints. Gentle exercise protects cartilage and supports flexibility.
- Know the red flags: swelling, stiffness, pain that won’t fade.
What Causes Sore Joints and How to Fix Them

Sore joints can come from [1] :
- Injuries
- Overuse or repetitive strain
- Arthritis and related conditions
It's possible to mix up sore joints with muscle soreness. Muscle pain usually eases with rest and is worse when moving, but joint soreness can persist even while resting. [2, 3]
Best Remedies for Sore Joints
- Heat and cold therapy - may reduce pain and swelling from an injury. [4]
- Rest - important to let the body heal, but prolonged inactivity can weaken your muscles and joints. [5, 23]
- OTC nonsteroidal anti-inflammatory drugs (like naproxen sodium, ibuprofen, or topical NSAIDs) - provides quick relief when needed, but avoid long-term, daily use. [6]
- 7-9 hours of deep sleep - critical for recovery and inflammation control. [7]
- Gut-friendly diet - a healthy diet reduces inflammation, helps relieve pressure on aching joints, and supports weight loss. [8]
- Targeted dietary supplements - Boswellia Serrata, collagen peptides, MSM, and curcumin+black pepper, plus fixing any nutrient deficiencies and imbalances such as vitamin D, magnesium, and omega-3s. [12]
If your pain comes from an injury or heavy strain, resting until pain subsides is important. However, in other cases, exercise and stretching are key; boosting circulation, protecting cartilage, and supporting joint resilience. [9, 10]
The Role of Joint Inflammation in Arthritis Pain

When joints are inflamed, pain is one of the main alarm signals. This goes away as the injury heals and inflammation fades. [13]
However, in rheumatoid arthritis (RA), the immune system stays switched on. Inflammation persists and the pain alarm doesn't turn off. [14]
This creates symptoms like:
- Swollen joints
- Stiff mornings
- Chronic pain, including when moving or doing daily activities
- Red and puffy hands
- Feeling drained
While arthritis doesn't pick age, it often starts between 30 and 60, with women 2-3 times more at risk. [14]
There's good news, though: not all joint inflammation or swelling means arthritis or another chronic disease. Sometimes it's just your body repairing itself due to an injury or sprain. These usually go away with rest and care.
- Inflammatory arthritis = system-wide inflammation that can cause chronic joint pain. Sprain or injury = often only local inflammation that disappears when the healing process finishes.
If you don't notice improvement after weeks of joint discomfort, it could signal something more serious, and means it's the time to call your MD.
Now, let's dive deeper into the soreness of specific joints, starting with the thumb.
Sore Thumb Relief
If your thumb is aching, it could be an injury, tendon strain, overuse, or arthritis. [15]
If the pain lingers, it's smart to get examined. Sometimes, an X-ray may be needed to diagnose a deeper issue.
Here's what can help:
- Splints - rest, protect, and stabilize your thumb, which can be especially useful at night.
- Anti-inflammatory creams - also called topical NSAIDs, you can rub these over the affected area for temporary relief. [16]
- Heat vs ice therapy - cold therapy (ice packs) in the first 24–48 hours. Then switch to a heating pad. [17]
- Rest - Give your thumb some downtime if the soreness comes from overuse or strain. But in the case of arthritis, activity is better than inactivity. [18]
Did you know? Texting thumb is real. It's related to excessive scrolling and typing, which can strain the joint. Stretching between sessions and limiting screen time if possible, can help. [19]
Sore Elbow Relief
Elbows feeling sore? The good news is, a lot of elbow pain can resolve with simple at-home care. It's often tendons overworked. [20]
Causes include tennis elbow, golfer's elbow, and strains. Activities like painting or using gripping tools can aggravate the problem. Step one is to ease up on movements that triggered it.
If your elbow is not just sore but also swollen, red, or hot to the touch, it could be a deeper issue that needs to be checked by a professional.
Let's say it's just a sore elbow: what can provide relief?
OTC anti-inflammatories can reduce pain short-term, but for lasting joint pain and inflammation support try gentle stretches, smart rest, targeted massage on specific points, and specialized joint supplements to help relieve joint pain and inflammation.
Did you know? Poor ergonomics at a computer can contribute to elbow pain as well as stress other joints. Adjust your desk set-up to keep elbows at a 90-degree angle, feet flat, and shoulders relaxed. [21]
Sore Hip Relief Without Complicated Treatments
Why do hips ache? Tight muscles, imbalances, osteoarthritis creeping in as cartilage gets compromised, or another inflammatory arthritis hurting the joint. [22]
Rest is key if you have sharp or injured hip pain. However, over-rest can weaken muscles and bones. [5, 23] As pain eases, start an exercise program or physical therapy that includes light stretching to maintain range of motion and strengthen muscles.
Don't forget the nutrition part. Olive oil, fish rich in omega-3 fatty acids, citrus fruits, and leafy greens contain compounds that help relieve inflammation and support collagen, which is crucial for joint maintenance. [24, 25, 26]
- Sitting for hours in a chair is a daily reality for many, but without proper breaks, training, or stretching, this can tighten your hip flexors and quietly stress your joints. [27, 28] A physical therapist can spot and address imbalances to fix your posture and relieve soreness.
Shoulder Joint Pain Relief Strategies
Due to their build and frequent use, shoulders are actually one of the most common sore joints. [29]
Potential causes range from improper training, overtraining, and awkward movements or twists, to arthritis (psoriatic, rheumatoid, or another type).
The relief strategy? Apply the same basics that work elsewhere. These include:
- Rest it
- Move it gently
- Ice first 24 hours, heat afterwards for another 24 hours
- Maintain proper posture by keeping your chest open and shoulders back
Shoulder pain heals slowly. Even mild pain can take several weeks or more. Pushing too soon can reset the clock, so arm yourself with patience. [30]
Big Toe Joint Pain Relief
Big toe joint pain can be sudden and intense, especially in gout, where the buildup of uric acid crystals triggers inflammation. [31]
Big toe soreness can also be caused by:
- Bunions - a bony bump at the base of the big toe, with swelling and pain worsening in tight shoes. [32]
- Hallux rigidus or hallux limitus - arthritis that wears down cartilage, leading to stiffness and discomfort due to bone rubbing against bone. [33]
- Overuse - repetitive strain or unaccustomed physical activity can spark inflammation of small bones under your big toe, causing sesamoiditis. [34]
If pain gets worse or persists, see your doctor. Meanwhile, rest, elevate, and ice 20 minutes on and off for 1-2 hours.
Other natural strategies to ease pain and soreness include:
- Big toe flexor stretches
- Picking right footwear (wide toe box wins over fashionable shoes that squeeze the foot)
- Avoid high-purine foods (red meat, beer), added sugars, and refined carbs like white bread and white rice; these are among the certain foods that can worsen inflammation.
- Tart cherries (50+ per day) or a supplement can aid joint relief. [35]
Everyday Habits To Manage Pain & Soreness (Anti-Inflammatory Foods, Fish Oil, and More)

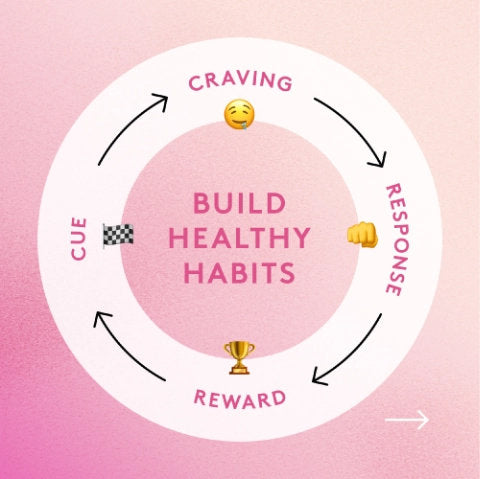
Regardless of which joint is giving you trouble, the following core habits can ease soreness and improve your comfort and mobility long-term:
- Regular movement - low-impact exercise like water aerobics keeps you staying active while building supportive muscles for joint comfort. It also gets joint fluid moving. [11]
- Maintain good posture - Poor ergonomics put extra pressure on joints. Sitting tall and opening your chest helps joints "breathe" easier.
- Nutrition over-haul - Foods that drive inflammation, such as fried seed oils, processed meat, refined carbs, and white sugar can worsen joint soreness, while foods that are high in anti-inflammatory omega-3s (fatty fish, chia seeds, algae oil supplements), antioxidants, and gut-healthy prebiotics (including 85% + dark chocolate, beans, barley, broccoli sprouts, garlic, and turmeric+black pepper) may support joint function and ease of movement. [26, 36, 37]
- Clinically-backed joint supplements - Boswellia Serrata, curcumin, glucosamine, and chondroitin have been studied for their potential to relieve pain and support connective tissue. Performance Lab® Flex delivers them in one clean, daily formula. [12]
Joint Pain or Arthritis Symptoms? When to See a Doctor
Mild sprain, overuse, or injury? These often heal with rest, light movement, and lifestyle fixes mentioned above.
But if you see swelling, stiffness, or severe pain that isn't improving, it indicates a deeper issue and need for medical evaluation.
If you're someone who likes to run but struggles with sore joints, the following article answers how you can protect your joints and move pain-free:
References
- MedlinePlus. (2024, June 24). Joint disorders. U.S. National Library of Medicine.
- NHS Inform. (2025, February 6). Pain and injuries after exercise (DOMS).
- MedlinePlus. (2024, March 31). Joint pain. U.S. National Library of Medicine.
- NHS. (n.d.). Joint pain.
- Kilroe, S. P., et al. (2020). Temporal muscle-specific disuse atrophy during one week of leg immobilization. *Medicine & Science in Sports & Exercise, 52*(9), 2067–2077.
- U.S. Food & Drug Administration. (2015). FDA strengthens warning that non-aspirin NSAIDs increase risk of heart attack or stroke. (Updated).
- National Sleep Foundation. (2020, October 1). How much sleep do you really need? *Sleep and You*.
- Sala-Climent, M., López de Coca, T., Guerrero, M. D., Muñoz, F. J., López-Ruíz, M. A., Moreno, L., Alacreu, M., & Dea-Ayuela, M. A. (2023). The effect of an anti-inflammatory diet on chronic pain: A pilot study. *Frontiers in Nutrition, 10*, 1205526.
- Kong, H., Wang, X. Q., & Zhang, X. A. (2022). Exercise for osteoarthritis: A literature review of pathology and mechanism. *Frontiers in Aging Neuroscience, 14*, 854026.
- Patel, P. N., Horenstein, M. S., & Zwibel, H. (2024, October 6). Exercise physiology. In *StatPearls*. StatPearls Publishing.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2024, May 15). Osteoarthritis of the knee: Learn more – What can you do to strengthen your knees? In *InformedHealth.org*. Institute for Quality and Efficiency in Health Care (IQWiG).
- Colletti, A., & Cicero, A. F. G. (2021). Nutraceutical approach to chronic osteoarthritis: From molecular research to clinical evidence. *International Journal of Molecular Sciences, 22*(23), 12920.
- U.S. National Library of Medicine. (2023, May 23). Ouch—That hurts: The science of pain. *MedlinePlus Magazine*.
- Cleveland Clinic. (2025). Rheumatoid arthritis: Overview and symptoms.
- American Society for Surgery of the Hand. (2021, February 1). 5 causes of thumb pain. *HandCare Blog*.
- Derry, S., Conaghan, P., Da Silva, J. A., Wiffen, P. J., & Moore, R. A. (2016). Topical NSAIDs for chronic musculoskeletal pain in adults. *The Cochrane Database of Systematic Reviews, 4*(4), CD007400.
- Ventriglia, G., Gervasoni, F., Franco, M., Magni, A., Panico, G., & Iolascon, G. (2023). Musculoskeletal pain management and thermotherapy: An exploratory analysis of Italian physicians’ attitude, beliefs, and prescribing habits. *Journal of Pain Research, 16*, 1547–1557.
- Cooney, J. K., Law, R. J., Matschke, V., Lemmey, A. B., Moore, J. P., Ahmad, Y., Jones, J. G., Maddison, P., & Thom, J. M. (2011). Benefits of exercise in rheumatoid arthritis. *Journal of Aging Research, 2011*, 681640.
- American Society for Surgery of the Hand. (n.d.). Gamer’s/Texter’s thumb: What is it? Symptoms, causes, treatment. *HandCare*.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2022, March 29). Tendon overuse injuries (tendinopathy): How are tendon overuse injuries treated? In *InformedHealth.org*.
- Kibria, M. G., Parvez, M. S., Saha, P., & Talapatra, S. (2023). Evaluating the ergonomic deficiencies in computer workstations and investigating their correlation with reported musculoskeletal disorders and visual symptoms among computer users in Bangladeshi university. *Heliyon, 9*(11), e22179.
- Chamberlain, R. (2021). Hip pain in adults: Evaluation and differential diagnosis. *American Family Physician, 103*(2), 81–89.
- Parry, S. M., & Puthucheary, Z. A. (2015). The impact of extended bed rest on the musculoskeletal system in the critical care environment. *Extreme Physiology & Medicine, 4*, 16.
- Zivkovic, A. M., Telis, N., German, J. B., & Hammock, B. D. (2011). Dietary omega-3 fatty acids aid in the modulation of inflammation and metabolic health. *California Agriculture, 65*(3), 106–111.
- Miles, E. A., & Calder, P. C. (2021). Effects of citrus fruit juices and their bioactive components on inflammation and immunity: A narrative review. *Frontiers in Immunology, 12*, 712608.
- Yu, X., Pu, H., & Voss, M. (2024). Overview of anti-inflammatory diets and their promising effects on non-communicable diseases. *The British Journal of Nutrition, 132*(7), 898–918.
- Yoo, W. G. (2014). Effect of resting in a chair, resting with range of motion exercises, and back strengthening exercises on pain and the flexion-relaxation ratio of computer workers with low back pain. *Journal of Physical Therapy Science, 26*(2), 321–322.
- Ehresman, B. A., Lehecka, B. J., Hiser, D., Koster, L., & Wietharn, J. (2025). Improved hip flexibility and gluteal function following a daily lunge-and-reach stretching intervention. *International Journal of Sports Physical Therapy, 20*(6), 814–823.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2024, April 22). Overview: Shoulder pain. In *InformedHealth.org*.
- Cadogan, A., Laslett, M., Hing, W. A., McNair, P. J., & Coates, M. H. (2011). A prospective study of shoulder pain in primary care: Prevalence of imaged pathology and response to guided diagnostic blocks. *BMC Musculoskeletal Disorders, 12*, 119.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). (2023, December). Gout: Symptoms, causes, & risk factors. NIAMS.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2024, October 9). Overview: Bunions. In *InformedHealth.org*.
- Lam, A., Chan, J. J., Surace, M. F., & Vulcano, E. (2017). Hallux rigidus: How do I approach it? *World Journal of Orthopedics, 8*(5), 364–371.
- Kaur, P., Carroll, M. R., & Stewart, S. (2023). The assessment and management of sesamoiditis: A focus group study of podiatrists in Aotearoa New Zealand. *Journal of Foot and Ankle Research, 16*(1), 29.
- Kelley, D. S., Adkins, Y., & Laugero, K. D. (2018). A review of the health benefits of cherries. *Nutrients, 10*(3), 368.
- Sibille, K. T., King, C., Garrett, T. J., Glover, T. L., Zhang, H., Chen, H., Reddy, D., Goodin, B. R., Sotolongo, A., Petrov, M. E., Cruz-Almeida, Y., Herbert, M., Bartley, E. J., Edberg, J. C., Staud, R., Redden, D. T., Bradley, L. A., & Fillingim, R. B. (2018). Omega-6: Omega-3 PUFA ratio, pain, functioning, and distress in adults with knee pain. *The Clinical Journal of Pain, 34*(2), 182–189.
- Gioia, C., Lucchino, B., Tarsitano, M. G., Iannuccelli, C., & Di Franco, M. (2020). Dietary habits and nutrition in rheumatoid arthritis: Can diet influence disease development and clinical manifestations? *Nutrients, 12*(5), 1456.