Running is one of the most enjoyable and effective ways to boost your health. [1, 2]
Research shows that exercises like running may relieve stress, support weight loss, and enhance energy levels. [3, 4, 5, 6]
But there's a problem: you have joint pain during or after running. Sometimes the pain is mild; other times, it's intense enough to limit your activity and daily life.
If this sounds familiar, you're not alone. Sore knees, hips, ankles, and other joints are known issues among runners. [7]
Hitting the pavement can either stress or support your joints—depending on factors like form, recovery, running surface, and nutrition. [8]
In this article, we'll explore:
- "Why your joints may hurt from running"
- "Expert-backed tips to manage soreness and reduce pain"
- "How to minimize your risk of joint pain and running injuries"
Let's get started!
Key Takeaways
- Running is great for overall health, but repetitive impact, poor form, and inadequate recovery can leave joints feeling sore and stiff.
- Common runner problems include knee pain, ankle sprains, plantar fasciitis, and iliotibial band syndrome from overloaded muscles and connective tissues.
- Good footwear, gradual training progressions, strength and mobility work, and proper warm-ups go a long way toward preventing joint pain.
- Listening to early warning signs and backing off when pain is sharp, localized, or persistent helps you avoid more serious injuries.
- Targeted recovery strategies, anti-inflammatory support, and smart programming make it easier to stay active and pain-free long term.

Is Running Bad or Good for Your Joints?

Let's start with this question: is running good or bad for your knees?
Since knees absorb a lot of impact when running, it's easy to assume that the activity can stress your joints over time.
However, it's the opposite. Research shows that moderate running may actually protect and strengthen your bones and joints. [9, 10, 11]
So why do some people feel like running is making their joints worse? Common sources include overuse (increasing mileage and intensity too quickly), poor form, muscle imbalances, conditions like scoliosis, nutrient deficiencies, and not listening to your body. [12, 13]
Many runners chase the feeling of a ‘runner’s high.’ However, regular running without taking breaks can cause wear and tear to connective tissues, including the Achilles tendon, over time. [14, 15]
The surfaces you run on matter, too. Softer terrains like grass, dirt, and woodland paths might be easier on your joints than hard surfaces like concrete. [8]
Is Running with Arthritis and Knee Pain Safe?

Patients with arthritis might wonder: "will running worsen my condition?".
The answer is, mild arthritis doesn't have to stop you from running. Assuming you do it in moderation and with proper form. In fact, exercise is one of the best natural treatments for osteoarthritis, and it may reduce the chance of developing arthritis in the first place. [12]
With that said, watch out for symptoms like stiffness, swelling, and pain behind the kneecap, in the feet, or in other joints after running. If they're persistent or severe, it might be an injury. Pain due to an injury can make it difficult to bear weight and should not be ignored. [16]
Common Joint Health Issues in Runners

Runners—especially those covering long distances—are no strangers to joint pain and injuries like shin splints, tendonitis, and a sprained ankle. This is often the result of repeated and excessive strain on the tendons, ligaments, feet, and other connective tissues. [7, 17]
Recognizing the specific joint issue you're dealing with is the first step toward treating it.
Common joint issues in runners include:
Runner's Knee
Patellofemoral pain syndrome, more often called runner's knee, is one of the most reported injuries in running. [18] This condition causes inflammation and pain beneath the kneecap (patella), in front of the knee. It can either be dull pain, or sharp and severe. [19]
Common causes of knee pain may include weak muscles, improper running form, and excess strain on the joint. [19]
-
Did you know? Experts suggest that women are twice as likely to report knee pain as men. [20, 21]
The best way to address runner's knee is to take a break until pain goes away. Afterwards, gradually introduce leg exercises that strengthen your supporting muscles. [22]
Runner's Hip
Runner's hip, or hip bursitis, is a term for pain and inflammation in the hip area. Common causes include overuse and muscle strain. [23, 24]
Symptoms include soreness around hip muscles that is usually mild and transient. However, persistent or severe pain might signal you're injured and need to take some time off.
Dealing with runner's hip comes down to fixing how your whole body moves, starting with your feet and hips. You should consider doing strengthening exercises, correcting muscle imbalances, and getting hands-on therapy to improve joint movement. [25]
Plantar Fasciitis
Plantar fasciitis is an inflammation of plantar fascia, the fibrous tissue that connects your heel bone to your toes. While not a joint, it plays a role in joint stress and foot biomechanics.
When you overstrain the plantar fascia—whether that's from long-distance running, standing on your feet the whole day, ankle instability, or excessive body weight—the tissue can become inflamed. [26, 27]
A classic symptom is heel pain. The pain is often sharp and occurs when you put weight on the heel, and especially after a period of inactivity. [28]
Dealing with this condition involves resting, putting ice on the affected area, and doing light stretching to aid recovery. [29, 30]
Iliotibial Band Syndrome (ITBS)
Iliotibial band is a thick band of connective tissue that runs along the outside of your thigh, connecting your hip to your knee.
Repetitive and straining activities like long-distance running can cause the band to rub against your hip and thigh bones, leading to irritation and sharp pain on the outside of the knee. [31]
Common causes of ITB may include weak hips or glutes, poor running form, and overuse. [32]
Prevention and treatment of ITB includes cryotherapy, strengthening your muscles, physical therapy, warming up with dynamic stretching before running, and avoiding overtraining on downhill runs. [33]
Is it Normal for my Joints to Hurt After Running?

Occasional mild soreness is normal, more so in new runners and those ramping up the intensity. Often, it's possible to mistake joint pain for muscle soreness. [34]
But persistent, sharp, or aggravating pain is not normal. Key distinction here is between soreness vs. injury. [35, 36]
If it's an injured joint, you may need a check-up by a specialist like an orthopaedic surgeon. This is especially important as we get older—runners often complain of more joint pains as they age, linked to weight gain and loss of cartilage. [37, 38]
How to Prevent Injury and Pain from Running

Running injuries can happen to anyone—regardless if you're an experienced runner or a beginner. The good news is, there are ways you can reduce the risk.
Evidence shows that the most important factor in preventing injuries is being careful to not overdo it with exercise and recognizing symptoms of overuse on time. [17]
Additionally, recovery training methods, stretching, and posture correction can help resolve early joint problems before they become more serious.
Here are some tips:
- Warm up with 5-10 minutes of brisk walking or gentle jogging.
- Dynamic stretching before a run prepares your muscles, ligaments, and tendons for movement.
- Cool down gradually by walking or lightly jogging for another 10 minutes before finishing.
- Static stretches after running are recommended for recovery and flexibility.
- Follow a structured plan to build up your running distance safely, if you're a beginner.
- Eat nutrient-dense, whole foods and consider supplements to aid joint health. [39, 40]
Also consider the following:
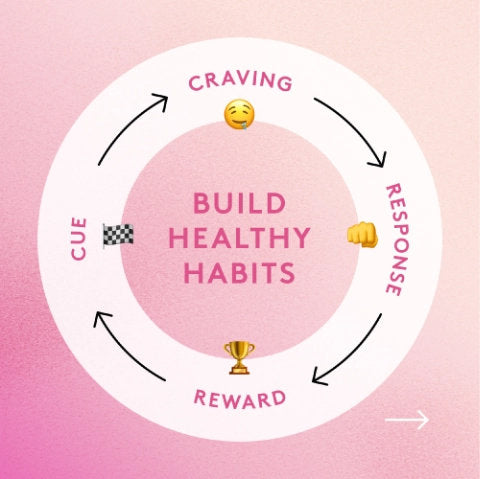
Listen to Your Body
Knowing when to take a break can help reduce injury risk while running. It's crucial that you don't ignore small pains or poor form. Track any symptoms and use apps or journals. [41]
Tip: track the frequency and duration of any pain. This can help you find out what's causing discomfort, and when it tends to happen.
Do Cross Training
Cross training involves doing exercises different from running, such as cycling, swimming, or strength training.
It strengthens your supporting muscles and joints, making your body more resilient to overuse injuries.
Wear Right Shoes
It's a common belief that wearing worn-down sneakers that have lost their cushioning may put excess strain on your ankles, heels, and feet. But what does the research actually say?
Surprisingly, a 2011 study titled "Are old running shoes detrimental to your feet? A pedobarographic study" found that brand new shoes can put more stress on your feet than well-worn ones. [42]
Researchers suggest this could be due to the stiffness of new materials, which haven't yet molded to your feet. Their advice? Break into new shoes gradually, using them for light activity at first.
On the other hand, a 2020 systematic review offered a deeper look into how shoe design might affect your feet and running experience[43]:
- Stiffer shoes (but not too stiff) can potentially help you go faster.
- Softer soles help absorb shock and protect the legs.
- Thicker soles give better cushioning, but make it harder to feel the ground.
- Minimalist, thin shoes can make running more efficient and strengthen your Achilles tendon, but they may also increase pressure on feet and ankles.
The takeaway? While research is limited, experts seem to agree on the following:
- Shoes that are completely worn out and have no cushioning are probably best avoided.
- It's wise to invest in proper shoes and get them fitted at a running shop—but make sure to get accustomed to them before putting in serious miles.
Managing and Recovering from Sore Joints After Running

Had a painful run? Here are some immediate steps you can take:
- Rest, ice, and compression. Doing this may promote healing and reduce swelling and pain. [44]
- Gentle mobility and stretching. Light recovery movements may support post-run comfort.
- Foam rolling and massage. Careful foam rolling can ease the soreness, while massage boosts muscle blood flow and lowers inflammation. [45, 46, 47]
Bonus tip: make sure your diet is topped up with whole foods rich in vitamin C and flavonoids, which may assist in the healing process. [48, 49]
How Long Does Joint Soreness From Running Last?
Mild muscle soreness after running can sometimes be mistaken for joint soreness. If you experience any pain after running, it should resolve within 2-5 days of a running session. [50] However, if it's truly joint pain from an injury, full recovery can take anywhere from a few weeks to several months, depending on the severity. [51]
Some people wonder, should you train at all if you have pain? Mild, achy pain that goes away as you warm up might be fine to push through. But if the pain gets worse, comes with swelling or limping, or lasts longer than a week, stop running and get advice from a specialized sports medicine provider who can guide your recovery.
How Supplements Can Assist Joint Recovery

If you're looking for an effective way to support joint health, supplements can be a valuable addition to your routine.
They may help to reduce inflammation, pain, and soreness from running, and feed your joints with nutrients needed for optimal recovery. [52, 53]
Enter Performance Lab® Flex.

Vegan-friendly and free of synthetic fillers, Performance Lab® Flex is made for runners and individuals who are looking to relieve soreness and protect their joints from everyday stress. It contains clinically-backed, anti-inflammatory ingredients like curcumin and AprèsFlex® Boswellia Serrata, which may ease joint stiffness from running. [54, 55, 56]
Its gentle ingredient dosages make it safe for daily use by anyone—from recovering runners to older adults looking to stay active.
For additional benefits, combine Performance Lab® Flex with Performance Lab® Omega-3. Together, they work to promote full-spectrum joint recovery and lasting comfort.
References
- Lee, D. C., et al. (2014). Leisure-time running reduces all-cause and cardiovascular mortality risk. JACC, 64(5), 472–481. https://doi.org/10.1016/j.jacc.2014.04.058
- Hespanhol Junior, L. C., Pillay, J. D., van Mechelen, W., & Verhagen, E. (2015). Meta-Analyses of the Effects of Habitual Running on Indices of Health in Physically Inactive Adults. Sports medicine (Auckland, N.Z.), 45(10), 1455–1468. https://doi.org/10.1007/s40279-015-0359-y
- Nowacka-Chmielewska, M., Grabowska, K., Grabowski, M., Meybohm, P., Burek, M., & Małecki, A. (2022). Running from Stress: Neurobiological Mechanisms of Exercise-Induced Stress Resilience. International journal of molecular sciences, 23(21), 13348. https://doi.org/10.3390/ijms232113348
- Jayedi, A., Soltani, S., Emadi, A., Zargar, M. S., & Najafi, A. (2024). Aerobic Exercise and Weight Loss in Adults: A Systematic Review and Dose-Response Meta-Analysis. JAMA network open, 7(12), e2452185. https://doi.org/10.1001/jamanetworkopen.2024.52185
- Wender, C. L. A., Manninen, M., & O'Connor, P. J. (2022). The Effect of Chronic Exercise on Energy and Fatigue States: A Systematic Review and Meta-Analysis of Randomized Trials. Frontiers in psychology, 13, 907637. https://doi.org/10.3389/fpsyg.2022.907637
- Hossain, M. N., Lee, J., Choi, H., Kwak, Y. S., & Kim, J. (2024). The impact of exercise on depression: how moving makes your brain and body feel better. Physical activity and nutrition, 28(2), 43–51. https://doi.org/10.20463/pan.2024.0015
- Kakouris, N., Yener, N., & Fong, D. T. P. (2021). A systematic review of running-related musculoskeletal injuries in runners. Journal of sport and health science, 10(5), 513–522. https://doi.org/10.1016/j.jshs.2021.04.001
- Tessutti, V., Ribeiro, A. P., Trombini-Souza, F., & Sacco, I. C. (2012). Attenuation of foot pressure during running on four different surfaces: asphalt, concrete, rubber, and natural grass. Journal of sports sciences, 30(14), 1545–1550. https://doi.org/10.1080/02640414.2012.713975
- Zhang, C., Wang, S., Meng, F., Shu, D., & Huang, H. (2025). Comparison of trabecular bone microarchitecture between older males with and without a running habit: A cross-sectional study. Journal of Exercise Science & Fitness. https://www.sciencedirect.com/science/article/pii/S1728869X25000024
- Garofolini, A., & Taylor, S. (2019). The effect of running on foot muscles and bones: A systematic review. Human Movement Science, 66, 585–595. https://www.sciencedirect.com/science/article/pii/S0167945718306092
- Lee, J. H. (2019). The effect of long-distance running on bone strength and bone biochemical markers. Journal of Exercise Rehabilitation, 15(1), 26–30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6416492/
- Lo, G. H., Driban, J. B., Kriska, A. M., McAlindon, T. E., & Eaton, C. B. (2017). Is there an association between recreational running and osteoarthritis? Journal of Orthopaedic & Sports Physical Therapy, 47(6), 391–398. https://doi.org/10.2519/jospt.2017.0505
- Correia, C. K., Machado, J. M., Dominski, F. H., de Castro, M. P., de Brito Fontana, H., & Ruschel, C. (2024). Risk factors for running-related injuries: An umbrella systematic review. Journal of sport and health science, 13(6), 793–804. https://doi.org/10.1016/j.jshs.2024.04.011
- Medina Pabón, M. A., & Naqvi, U. (2025, January). Achilles tendinopathy. In StatPearls [Internet]. StatPearls Publishing. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK538149/
- Lagas, I. F., Fokkema, T., Verhaar, J. A. N., Bierma-Zeinstra, S. M. A., van Middelkoop, M., & de Vos, R. J. (2020). Incidence of Achilles tendinopathy and associated risk factors in recreational runners: A large prospective cohort study. Journal of science and medicine in sport, 23(5), 448–452. https://doi.org/10.1016/j.jsams.2019.12.013
- Elsevier. (n.d.). Ligament injury. In ScienceDirect Topics. Retrieved June 8, 2025, from https://www.sciencedirect.com/topics/medicine-and-dentistry/ligament-injury
- van Mechelen W. (1992). Running injuries. A review of the epidemiological literature. Sports medicine (Auckland, N.Z.), 14(5), 320–335. https://doi.org/10.2165/00007256-199214050-00004
- Kakouris, N., Yener, N., & Fong, D. T. P. (2021). A systematic review of running-related musculoskeletal injuries in runners. Journal of sport and health science, 10(5), 513–522. https://doi.org/10.1016/j.jshs.2021.04.001
- Institute for Quality and Efficiency in Health Care (IQWiG). (2024, January 30). Overview: Patellofemoral pain syndrome (runner’s knee). In InformedHealth.org [Internet]. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK561507/
- Francis, P., Whatman, C., Sheerin, K., Hume, P., & Johnson, M. I. (2019). The Proportion of Lower Limb Running Injuries by Gender, Anatomical Location and Specific Pathology: A Systematic Review. Journal of sports science & medicine, 18(1), 21–31.
- Boling, M., Padua, D., Marshall, S., Guskiewicz, K., Pyne, S., & Beutler, A. (2010). Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scandinavian Journal of Medicine & Science in Sports, 20(5), 725–730. https://doi.org/10.1111/j.1600-0838.2009.00996.x
- Institute for Quality and Efficiency in Health Care (IQWiG). (2024, January 30). Patellofemoral pain syndrome (runner’s knee): Learn more – How can you relieve pain at the front of the knee? In InformedHealth.org [Internet]. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK561504/
- Seidman, A. J., Taqi, M., & Varacallo, M. A. (2025, January). Trochanteric bursitis [Archived]. In StatPearls [Internet]. StatPearls Publishing. Retrieved June 8, 2025, from https://pubmed.ncbi.nlm.nih.gov/30860738/
- Paluska S. A. (2005). An overview of hip injuries in running. Sports medicine (Auckland, N.Z.), 35(11), 991–1014. https://doi.org/10.2165/00007256-200535110-00005
- Geraci, M. C., Jr, & Brown, W. (2005). Evidence-based treatment of hip and pelvic injuries in runners. Physical medicine and rehabilitation clinics of North America, 16(3), 711–747. https://doi.org/10.1016/j.pmr.2005.02.004
- Riddle, D. L., et al. (2003). Risk factors for plantar fasciitis: A matched case-control study. The Journal of Bone and Joint Surgery. American Volume, 85(5), 872–877. https://doi.org/10.2106/00004623-200305000-00015
- Allam AE, Chang KV. Plantar Heel Pain. [Updated 2024 Jan 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499868/
- Neufeld, S. K., & Cerrato, R. A. (2008). Plantar fasciitis: Evaluation and treatment. Journal of the American Academy of Orthopaedic Surgeons, 16(6), 338–346. https://doi.org/10.5435/00124635-200806000-00006
- Buchanan, B. K., Sina, R. E., & Kushner, D. (2025, January). Plantar fasciitis. In StatPearls [Internet]. StatPearls Publishing. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK431073/
- Lim, A. T., How, C. H., & Tan, B. (2016). Management of plantar fasciitis in the outpatient setting. Singapore medical journal, 57(4), 168–171. https://doi.org/10.11622/smedj.2016069
- Fairclough, J., et al. (2006). The functional anatomy of the iliotibial band during flexion and extension of the knee: Implications for understanding IT band syndrome. Journal of Anatomy, 208(3), 309–316. https://doi.org/10.1111/j.1469-7580.2006.00531.x
- Fredericson, M., & Wolf, C. (2005). Iliotibial band syndrome in runners: innovations in treatment. Sports medicine (Auckland, N.Z.), 35(5), 451–459. https://doi.org/10.2165/00007256-200535050-00006
- Hadeed, A., & Tapscott, D. C. (2025, January). Iliotibial band friction syndrome. In StatPearls [Internet]. StatPearls Publishing. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK542185/
- Vickers A. J. (2001). Time course of muscle soreness following different types of exercise. BMC musculoskeletal disorders, 2, 5. https://doi.org/10.1186/1471-2474-2-5
- DeYulis, M., & Hinson, J. W. (2025, January 14). Joint immobilization. In StatPearls [Internet]. StatPearls Publishing. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK557703/
- Havelin, J., & King, T. (2018). Mechanisms Underlying Bone and Joint Pain. Current osteoporosis reports, 16(6), 763–771. https://doi.org/10.1007/s11914-018-0493-1
- Molina, J., & Morgan, E. L. (2025, January). Obesity and orthopedic issues. In StatPearls [Internet]. StatPearls Publishing. Retrieved June 8, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK572101/
- Li, Y., Wei, X., Zhou, J., & Wei, L. (2013). The age-related changes in cartilage and osteoarthritis. BioMed research international, 2013, 916530. https://doi.org/10.1155/2013/916530
- Clark K. L. (2007). Nutritional considerations in joint health. Clinics in sports medicine, 26(1), 101–118. https://doi.org/10.1016/j.csm.2006.11.006
- Paultre, K., Cade, W., Hernandez, D., Reynolds, J., Greif, D., & Best, T. M. (2021). Therapeutic effects of turmeric or curcumin extract on pain and function for individuals with knee osteoarthritis: a systematic review. BMJ open sport & exercise medicine, 7(1), e000935. https://doi.org/10.1136/bmjsem-2020-000935
- Linton, L., Culpan, J., & Lane, J. (2025). Running-Centred Injury Prevention Support: A Scoping Review on Current Injury Risk Reduction Practices for Runners. Translational sports medicine, 2025, 3007544. https://doi.org/10.1155/tsm2/3007544
- Rethnam, U., & Makwana, N. (2011). Are old running shoes detrimental to your feet? A pedobarographic study. BMC research notes, 4, 307. https://doi.org/10.1186/1756-0500-4-307
- Sun, X., Lam, W. K., Zhang, X., Wang, J., & Fu, W. (2020). Systematic Review of the Role of Footwear Constructions in Running Biomechanics: Implications for Running-Related Injury and Performance. Journal of sports science & medicine, 19(1), 20–37. https://pmc.ncbi.nlm.nih.gov/articles/PMC7039038/
- Bleakley, C. M., Glasgow, P., & MacAuley, D. C. (2012). PRICE needs updating, should we call the POLICE? British Journal of Sports Medicine, 46(4), 220–221. https://doi.org/10.1136/bjsports-2011-090297
- Cheatham, S. W., Kolber, M. J., Cain, M., & Lee, M. (2015). THE EFFECTS OF SELF-MYOFASCIAL RELEASE USING A FOAM ROLL OR ROLLER MASSAGER ON JOINT RANGE OF MOTION, MUSCLE RECOVERY, AND PERFORMANCE: A SYSTEMATIC REVIEW. International journal of sports physical therapy, 10(6), 827–838. https://pmc.ncbi.nlm.nih.gov/articles/PMC4637917/
- Weerapong, P., Hume, P. A., & Kolt, G. S. (2005). The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports medicine (Auckland, N.Z.), 35(3), 235–256. https://doi.org/10.2165/00007256-200535030-00004
- White, G. E., West, S. L., Caterini, J. E., Di Battista, A. P., Rhind, S. G., & Wells, G. D. (2020). Massage Therapy Modulates Inflammatory Mediators Following Sprint Exercise in Healthy Male Athletes. Journal of functional morphology and kinesiology, 5(1), 9. https://doi.org/10.3390/jfmk5010009
- Oakes, B., Bolia, I. K., Weber, A. E., & Petrigliano, F. A. (2021). Vitamin C in orthopedic practices: Current concepts, novel ideas, and future perspectives. Journal of orthopaedic research : official publication of the Orthopaedic Research Society, 39(4), 698–706. https://doi.org/10.1002/jor.24947
- Al-Khayri, J. M., Sahana, G. R., Nagella, P., Joseph, B. V., Alessa, F. M., & Al-Mssallem, M. Q. (2022). Flavonoids as Potential Anti-Inflammatory Molecules: A Review. Molecules (Basel, Switzerland), 27(9), 2901. https://doi.org/10.3390/molecules27092901
- Vickers A. J. (2001). Time course of muscle soreness following different types of exercise. BMC musculoskeletal disorders, 2, 5. https://doi.org/10.1186/1471-2474-2-5
- Button, K., van Deursen, R., & Price, P. (2005). Measurement of functional recovery in individuals with acute anterior cruciate ligament rupture. British journal of sports medicine, 39(11), 866–871. https://doi.org/10.1136/bjsm.2005.019984
- Liu, X., Machado, G. C., Eyles, J. P., Ravi, V., & Hunter, D. J. (2018). Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. British journal of sports medicine, 52(3), 167–175. https://doi.org/10.1136/bjsports-2016-097333
- Yu, G., Xiang, W., Zhang, T., Zeng, L., Yang, K., & Li, J. (2020). Effectiveness of Boswellia and Boswellia extract for osteoarthritis patients: a systematic review and meta-analysis. BMC complementary medicine and therapies, 20(1), 225. https://doi.org/10.1186/s12906-020-02985-6
- Peng, Y., Ao, M., Dong, B., Jiang, Y., Yu, L., Chen, Z., Hu, C., & Xu, R. (2021). Anti-Inflammatory Effects of Curcumin in the Inflammatory Diseases: Status, Limitations and Countermeasures. Drug design, development and therapy, 15, 4503–4525. https://doi.org/10.2147/DDDT.S327378
- Sakul, A. A., Balcikanli, Z., Ozsoy, N. A., Orhan, C., Sahin, N., Tuzcu, M., Juturu, V., Kilic, E., & Sahin, K. (2024). A highly bioavailable curcumin formulation ameliorates inflammation cytokines and neurotrophic factors in mice with traumatic brain injury. Chemical biology & drug design, 103(1), e14439. https://doi.org/10.1111/cbdd.14439
- Jamwal R. (2018). Bioavailable curcumin formulations: A review of pharmacokinetic studies in healthy volunteers. Journal of integrative medicine, 16(6), 367–374. https://doi.org/10.1016/j.joim.2018.07.001