Vitamin A does far more than just protect your eyes; it also affects your immune system, skin, hormones, and bones and joints. It has even been studied in conditions like lung cancer. [1, 2, 3, 30]
Your need for this nutrient rises during physiological stress and infections, and it's important to get enough through diet. [4, 5]
But the saying "too much of a good thing is bad" also applies to vitamin A. In fact, your joints might actually feel worse from overdoing it.
So, does vitamin A help painful joints, or make them worse? Let's break it down.
Key Takeaways
- Vitamin A is involved in immunity, bone health, and inflammation.
- It’s not a common fix for joint pain. Deficiency is rarely the culprit.
- Too much vitamin A can actually contribute to joint and bone pain.
- Keep it balanced. Safe levels support health, while excess risks toxicity.
- Other vitamins (D, C, K) and minerals (calcium, magnesium) are more directly linked to joint comfort.
Vitamin A & Joint Health — What Research Shows

Vitamin A has anti-inflammatory properties. [6] It helps to reduce cytokines (pro-inflammatory molecules) and support your immune balance. [7] Not getting enough vitamin A can elevate inflammation. [8, 9]
As inflammation is behind many types of joint pain, e.g. rheumatoid arthritis, it's natural to assume that vitamin A can help ease pain.
Except that the research doesn't confirm this; its anti-inflammatory effects, while important for systemic health, don't really translate to targeted joint pain relief. One national study even found that beyond a certain limit, vitamin A "becomes a causative factor for osteoarthritis." [10]
Cartilage and Bone Connection
While vitamin A doesn't aid joint pain directly, it's needed for bone formation and remodeling of bone tissue. [11] This is important because bones, joints, and cartilage are all deeply connected and affect each other.
As we've gone over earlier, the problem arises when there's excessive intake of vitamin A, potentially leading to side effects.
For example, a 2024 Frontiers in Endocrinology study found that excess vitamin A weakened animal bones by shrinking cortical bone, slowing formation, and speeding up bone resorption. [12]
On the other hand, maintaining healthy levels of vitamin A has been shown to benefit bone strength and function. [34]
For joint function, vitamin A interacts with other fat-soluble vitamins. These include:
- Vitamin D - affects bone density and calcium absorption [13]
- Vitamin E - shields fats and cell membranes from oxidative stress [14]
- Vitamin K - directs calcium to bones instead of joints or arteries [15]
The key to comprehensive support is consuming a diversity of nutrients rather than just taking vitamin A on its own. [16, 17]
You Might Also Like: Best Vitamins for Bone and Joint Health
Does Too Much Vitamin A Cause Joint Pain?

The answer is: yes, it can. Joint and bone pain is one of the potential symptoms of vitamin A toxicity (also called hypervitaminosis A). [18]
Being fat-soluble, vitamin A is stored primarily in your liver. If you take high doses from dietary supplements or foods like beef liver, it can rise to dangerous levels.
Toxicity symptoms include:
- Joint and bone pain
- Headaches and dizziness
- Dry skin and hair loss
- Liver damage
- Blurry vision
Pregnant women should be especially careful with vitamin A intake, as excess is linked to birth defects. [32]
If you experience joint pain and are taking vitamin A supplements, it's worth ruling out toxicity by getting tested by your doctor.
What Vitamin Might You Be Lacking If Your Joints Hurt?

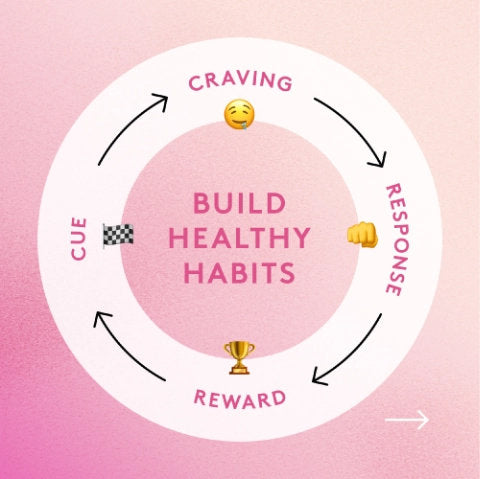
So, vitamin A deficiency is not the usual suspect if you have joint pain. The more likely reasons include an injury, strain, viral infections, and arthritis types (gout, RA, OA, etc.). [19]
Figuring out the cause of joint pain helps you find the most effective solution. For example, in gout, joint pain happens as a result of uric acid crystals building up in joints, so lowering uric acid levels provides symptom relief. [31]
That said, joint pain can be affected by nutrient deficiencies. These include: [20, 21, 22, 23, 24, 25]:
- Vitamin D: deficiency has been linked to joint pain and weakness.
- Vitamin C: not getting enough can disturb collagen synthesis in cartilage and connective tissue.
- Vitamin K: a lack of this nutrient may interfere with proper bone mineralization.
- Calcium & Magnesium: without these foundational minerals, nerve and muscle function as well as skeletal health get compromised.
Tip: if you suspect a deficiency, make sure to rule out any underlying condition.
Signs of Vitamin A Deficiency
Vitamin A is found in vitamin A-rich foods like eggs, fish, liver, and other animal products, as well as in the form of beta-carotene in carrots, sweet potatoes, and pumpkins. [18] Other concentrated sources include fish liver oils commonly taken as supplements. Deficiency is not common in the U.S. [26]
Still, that doesn't mean it can't occur. Two big signs to watch out for are night blindness and frequent infections. Vitamin A also plays a role in healthy cell growth, which is why deficiency can slow wound healing. [33]
In really severe cases, vision loss and keratinization of tissues (patches of skin becoming hard and rough) can occur. [29]
Can Vitamin A Help Rheumatoid Arthritis Symptoms?

Many people with arthritis reach for nonsteroidal anti-inflammatory drugs (NSAIDs) to manage symptoms.
Others, concerned about potential side effects of these drugs, look for natural vitamins to ease pain and discomfort, with some nutrients being more helpful than others. Vitamin A seems to belong to the latter category.
Human studies on vitamin A easing arthritis are limited, though some animal research points to potential benefits.
A 2024 research article in Scientific Reports found how all-trans retinoic acid (ATRA), a vitamin A metabolite, helped to support immune and gut health to counter arthritis symptoms in rats.
It dampened arthritis symptoms by recalibrating immune balance (Th17 vs Treg), reducing inflammation, and reinforcing gut barrier integrity.
What's more, ATRA improved the animal's internal ecosystem by shifting gut bacteria away from harmful strains and toward gut-supportive Lactobacilli. [27]
Needless to say, the study used a specific metabolite of vitamin A in specific doses, and only in animals. It remains to be seen how this translates to vitamin A from foods and supplements in humans.
The bottom line is: Vitamin A looks to be a potentially supportive, but not primary nutrient in arthritis management.
Is 2,000 mcg Vitamin A Too Much?

The RDA for vitamin A is 700 mcg in women and 900 mcg in men. Upper limit is 3,000 mcg per day. Therefore, 2,000 mcg of vitamin A, while above the recommended dietary allowance, is still not above the upper limit. [28]
This dose might be safe short term, but the risk grows if sustained or combined with a high vitamin A diet. To be on the safe side, avoid taking higher-than-RDA doses (unless otherwise told by your doctor), especially if you experience joint pain.
Final Thoughts
Vitamin A's role in joint health is complex. While it's important for inflammation and bone growth, a deficiency is rarely linked to joint pain. And excess is.
Too much vitamin A contributes to increased risk of bone problems, liver damage, and other health issues.
NutriGenesis® Multi + Flex for Safe, Daily Joint Support

Steer clear of high-dose supplements and eat a healthy diet to get all the micronutrients. You can fill in any gaps with clean, well-absorbed forms of vitamins, like those in NutriGenesis® Multi.

For targeted joint support, Performance Lab® Flex supplies research-backed nutrients and plant extracts in safe, daily doses.
References
- Brossaud, J., Pallet, V., & Corcuff, J.-B. (2017). Vitamin A, endocrine tissues and hormones: Interplay and interactions. Endocrine Connections, 6(7), R121–R130. https://doi.org/10.1530/EC-17-0101
- Roche, F. C., & Harris-Tryon, T. A. (2021). Illuminating the role of vitamin A in skin innate immunity and the skin microbiome: A narrative review. Nutrients, 13(2), 302. https://doi.org/10.3390/nu13020302
- Yee, M. M. F., et al. (2021). Vitamin A and bone health: A review on current evidence. Molecules, 26(6), 1757. https://doi.org/10.3390/molecules26061757
- Stephensen, C. B., & Gildengorin, G. (2000). Serum retinol, the acute-phase response, and misclassification of vitamin A status in NHANES III. American Journal of Clinical Nutrition, 72(5), 1170–1178. https://doi.org/10.1093/ajcn/72.5.1170
- Rubin, L. P., et al. (2017). Metabolic effects of inflammation on vitamin A and carotenoid metabolism. Advances in Nutrition, 8(2), 197–212. https://doi.org/10.3945/an.116.014167
- Huang, Z., Liu, Y., Qi, G., Brand, D., & Zheng, S. G. (2018). Role of vitamin A in the immune system. Journal of Clinical Medicine, 7(9), 258. https://doi.org/10.3390/jcm7090258
- Mucida, D., Park, Y., Kim, G., et al. (2007). Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science, 317(5835), 256–260. https://doi.org/10.1126/science.1145697
- Stephensen, C. B. (2001). Vitamin A, infection, and immune function. Annual Review of Nutrition, 21, 167–192. https://doi.org/10.1146/annurev.nutr.21.1.167
- Gholizadeh, M., Basafa Roodi, P., Abaj, F., Shab-Bidar, S., Saedisomeolia, A., Asbaghi, O., & Lak, M. (2022). Influence of Vitamin A supplementation on inflammatory biomarkers in adults: a systematic review and meta-analysis of randomized clinical trials. Scientific reports, 12(1), 21384. https://pmc.ncbi.nlm.nih.gov/articles/PMC9735279
- Wu, A., Wu, N. N., Xu, P. H., Jin, Y., Yang, Z. K., & Teng, J. W. (2024). Association of blood vitamin A with osteoarthritis: a nationally representative cross-sectional study. Frontiers in nutrition, 11, 1459332. https://pmc.ncbi.nlm.nih.gov/articles/PMC11573514/
- Yee, M. M. F., et al. (2021). Vitamin A and bone health: A review on current evidence. Molecules, 26(6), 1757. https://doi.org/10.3390/molecules26061757
- Lerner, U. H. (2024). Vitamin A – Discovery, metabolism, receptor signaling and effects on bone mass and fracture susceptibility. Frontiers in Endocrinology, 15, Article 1298851. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1298851/full
- Holick, M. F. (2007). Vitamin D deficiency. New England Journal of Medicine, 357(3), 266–281. https://doi.org/10.1056/NEJMra070553
- Traber, M. G., & Atkinson, J. (2007). Vitamin E, antioxidant and nothing more? Free Radical Biology and Medicine, 43(1), 4–15. https://doi.org/10.1016/j.freeradbiomed.2007.03.024
- Shearer, M. J., & Newman, P. (2008). Metabolism and cell biology of vitamin K. Thrombosis and Haemostasis, 100(4), 530–547. https://doi.org/10.1160/TH08-03-0147
- Muñoz-Garach, A., García-Fontana, B., & Muñoz-Torres, M. (2020). Nutrients and Dietary Patterns Related to Osteoporosis. Nutrients, 12(7), 1986. https://doi.org/10.3390/nu12071986
- Mathieu, S., Soubrier, M., Peirs, C., Monfoulet, L. E., Boirie, Y., & Tournadre, A. (2022). A Meta-Analysis of the Impact of Nutritional Supplementation on Osteoarthritis Symptoms. Nutrients, 14(8), 1607. https://doi.org/10.3390/nu14081607
- Olson, J. M., Ameer, M. A., & Goyal, A. (2023, September 2). Vitamin A toxicity. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532916/
- Havelin, J., & King, T. (2018). Mechanisms Underlying Bone and Joint Pain. Current osteoporosis reports, 16(6), 763–771. https://pmc.ncbi.nlm.nih.gov/articles/PMC6554716/
- Laslett, L. L., Quinn, S., Burgess, J. R., Parameswaran, V., Winzenberg, T. M., Jones, G., & Ding, C. (2014). Moderate vitamin D deficiency is associated with changes in knee and hip pain in older adults: a 5-year longitudinal study. Annals of the rheumatic diseases, 73(4), 697–703. https://doi.org/10.1136/annrheumdis-2012-202831
- Cloney, K., Ramsey, S., & Burns, E. (2022). Vitamin C deficiency in a 12-year-old male presenting with knee pain: a case report. CJEM, 24(5), 544–546. https://pmc.ncbi.nlm.nih.gov/articles/PMC9081961/
- Zimmerman, L., Anastasopoulou, C., & McKeon, B. (2024, September 2). Osteomalacia. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551616/
- Veronese, N., La Tegola, L., Caruso, M. G., Maggi, S., & Guglielmi, G. (2019). The Association between Dietary Magnesium Intake and Magnetic Resonance Parameters for Knee Osteoarthritis. Nutrients, 11(6), 1387. https://doi.org/10.3390/nu11061387
- Shmagel, A. K., Onizuka, N., Langsetmo, L., Vo, T. N., Foley, R., Ensrud, K. E., & Valen, P. (2018). Low magnesium intake is associated with increased knee pain in subjects with radiographic knee osteoarthritis: Data from the Osteoarthritis Initiative. Osteoarthritis and Cartilage, 26(5), 651–658. https://doi.org/10.1016/j.joca.2018.02.002
- Misra, D., Booth, S. L., Tolstykh, I., Felson, D. T., Nevitt, M. C., Lewis, C. E., Torner, J., & Neogi, T. (2013). Vitamin K deficiency is associated with incident knee osteoarthritis. The American journal of medicine, 126(3), 243–248. https://doi.org/10.1016/j.amjmed.2012.10.011
- Hodge, C., & Taylor, C. (2023, January 2). Vitamin A deficiency. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK567744/
- Zhang, Y., Luo, Y., Shi, J., Xie, Y., Shao, H., & Li, Y. (2024). All-trans retinoic acid alleviates collagen-induced arthritis and promotes intestinal homeostasis. Scientific Reports, 14, Article 1811.
- Institute of Medicine (US) Panel on Micronutrients. (2001). Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK222318/
- Polcz, M. E., & Barbul, A. (2019). The Role of Vitamin A in Wound Healing. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition, 34(5), 695–700. https://doi.org/10.1002/ncp.10376
- Sun, Y., Wu, J., Yoon, H. S., Buchowski, M. S., Cai, H., Deppen, S. A., Steinwandel, M. D., Zheng, W., Shu, X. O., Blot, W. J., & Cai, Q. (2022). Associations of Dietary Intakes of Carotenoids and Vitamin A with Lung Cancer Risk in a Low-Income Population in the Southeastern United States. Cancers, 14(20), 5159. https://doi.org/10.3390/cancers14205159
- Engel, B., Just, J., Bleckwenn, M., & Weckbecker, K. (2017). Treatment Options for Gout. Deutsches Arzteblatt international, 114(13), 215–222. https://doi.org/10.3238/arztebl.2017.0215
- Abadie, R. B., Staples, A. A., Lauck, L. V., Dautel, A. D., Spillers, N. J., Klapper, R. J., Hirsch, J. D., Varrassi, G., Ahmadzadeh, S., Shekoohi, S., & Kaye, A. D. (2023). Vitamin A-Mediated Birth Defects: A Narrative Review. Cureus, 15(12), e50513. https://doi.org/10.7759/cureus.50513
- Chow, O., & Barbul, A. (2014). Immunonutrition: Role in Wound Healing and Tissue Regeneration. Advances in wound care, 3(1), 46–53. https://doi.org/10.1089/wound.2012.0415
- Ling L. (2025). Association between serum vitamin A and bone mineral density in adolescents. Scientific reports, 15(1), 6892. https://pubmed.ncbi.nlm.nih.gov/40011496/