Potassium is an essential mineral that supports muscle function, fluid levels, blood pressure, and nerve signals. Prolonged fasts can quickly deplete potassium levels, leading to symptoms like insomnia, headaches, dizziness, muscle spasms, fatigue, and even arrhythmias.
Whether you’ve experienced a painful night of leg cramps or seeing stars when you stand up too fast, chances are you’ve suffered from an electrolyte balance in some form. Be it during or after a prolonged fast, supplementing with electrolytes is critical to ensuring optimal function when energy intake stops.
While potassium isn’t the only essential mineral you should supplement while fasting, we’re giving you the details on why it’s important and where to find it.
Let’s get started.
Key Takeaways
- Electrolytes matter during fasting—potassium helps maintain nerve, muscle and cardiac function.
- Supplementing small, regular amounts can ease headaches, fatigue and cramping in longer fasts.
- Don’t combine with very high sodium without monitoring; keep fluids steady.
- People on kidney meds or with renal issues should consult a clinician first.
- Use clean, measured forms and avoid sugary electrolyte drinks to stay fasted.

What is Potassium?
Before we dive into everything you want to know about potassium and why it’s important to supplement during periods of low energy intake, we first need to ensure you have a solid foundation—what is potassium?
When you think about potassium, chances are a banana comes to mind. It’s one (but not the only) source of potassium in the diet.
Potassium is an essential mineral present in many foods that plays an integral role in the nervous system, as well as in muscle contractions, fluid balance, blood pressure, and more.
But despite its importance and dietary prevalence, it’s one of the four most common nutrient shortfalls in the American diet 1.
Potassium intake requirements increased in 2004 to 4700 mg/day, making it difficult for most Americans to achieve these levels. Americans consume just over half of the required amount, averaging 2591 mg daily.
But why should we care? Sufficient potassium intake is necessary for heart and bone health, cardiovascular function, and prevention of chronic diseases like stroke and coronary heart disease.
Along with potassium, we also have to consider the other electrolytes—sodium, magnesium, and calcium. These are all minerals critical to optimal health and well-being.
Not consuming enough during fasting, especially a prolonged fast, could lead to an electrolyte imbalance, quickly becoming life-threatening when left unchecked.
Related Post: Should I Take Potassium in the Morning or Night?
What Does Potassium Do?
So, why is potassium important?
The primary role of potassium is as an electrolyte. Not familiar with what electrolytes are? Technically, electrolytes are substances that dissociate in solution and can conduct an electrical current 2.
They are located in both intra- and extracellular fluid, with each location in the cell having a higher concentration of a specific electrolyte.
In extracellular fluid, the major cation is sodium, and the major anion is chloride, while potassium is the major cation in intracellular fluid. As a group, they play an essential role in maintaining homeostasis.
But there are more than just three:
- Sodium
- Potassium
- Chloride
- Calcium
- Magnesium
- Phosphate
- Bicarbonate
Although potassium has its health benefits, when we’re talking about it here, we are referring to its function as an electrolyte.
Here’s a breakdown of why we need potassium and other electrolytes:
1. Nervous system function
Your central nervous system controls your entire body, and when your brain sends signals out, they travel through nerve cells (neurons) to communicate to cells in other areas of the body.
These signals are called nerve impulses and are generated by changes in the electrical charge (voltage) of cell membranes 3.
The change in polarization of the membrane happens due to the movement of electrolytes across the cell membrane, which sets off a chain of events that moves sodium along the length of the nerve cell axon and allows the impulse to reach its final destination.
2. Muscle contraction
Whether you’re walking, lifting weights, sitting in a chair, or typing on a laptop, electrolytes are responsible for causing your muscles to contract—calcium, specifically 4.
A muscle contraction occurs when muscle filaments (actin and myosin) slide past one another via cross-bridges formed between the two 5.
When these cross-bridges are formed, it results in a tight contraction. Then, magnesium binds and changes the conformation of the cross-bridge, causing the linkage to weaken and detach, thereby relaxing the muscle.
Simply put, calcium binds to specific proteins in the muscle, resulting in changes to the protein’s shape and generating a contraction.
Because magnesium is a calcium antagonist, it competes for the same binding sites as calcium to induce muscle relaxation 6.
3. Hydration and fluid balance
The human body comprises roughly 60% water, 40% of which is found inside cells as intracellular fluid (ICF) 7. The remainder is located outside cells as blood, spinal fluid, and between cells as extracellular fluid (ECF).
The amount of water in the ICF and ECF is dictated by the concentration of electrolytes, specifically sodium and potassium.
Potassium determines the amount of water inside cells, while sodium determines the amount outside cells. Changes in either concentration can lead to fluid imbalances, which leads to cells shrinking or swelling 8.
Improper fluid balance can lead to dehydration, seriously impacting your organs, especially the heart and kidneys.
4. pH balance
Your body requires a specific pH to function optimally and maintains it within a very narrow range 9. In the body, pH is maintained by various chemical buffers that work to minimize changes in the acid-base balance of your internal environment.
For example, blood is maintained within a pH of 7.35 to 7.45; any deviation from this can have serious consequences. Having sufficient electrolytes is fundamental to maintaining the proper pH in the body.
But here’s the thing: potassium levels are rapidly depleted within the early stages of fasting and begin to taper off and level out. So, if you’re doing an extended fast and not replacing potassium, it can lead to serious imbalances.
What You Need To Know About Fasting And Electrolytes
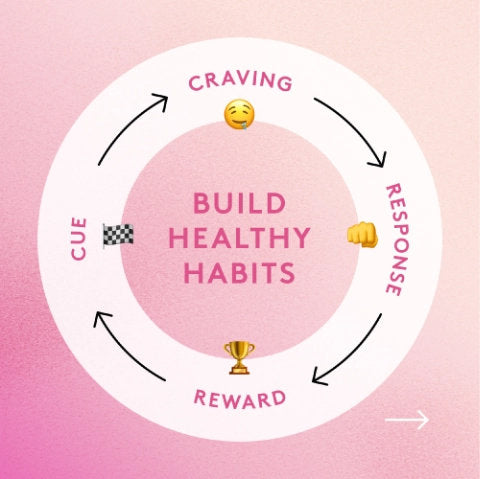
There are several reasons for an electrolyte imbalance: an unhealthy diet, excessive sweating, dehydration or overhydration, vomiting, illness, low-carb diets, and, of course, fasting.
But while electrolyte imbalances because of intense physical exertion is easy to understand (you’re losing a lot of sweating), it might be harder to wrap your head around how electrolyte happens with fasting.
In short, the longer the fast, the more electrolytes are released through urine, especially potassium and sodium 10.
And if you’re exercising during a fast, you can increase the loss of electrolytes, leading to a more pronounced imbalance.
So, it’s easy to see why if you’re not hydrating and replacing critical minerals, it’s easy for an imbalance to develop.
As a good rule of thumb, any fast longer than 12 hours could lead to an electrolyte deficiency. The body does have a small reserve of electrolytes, but these are typically depleted within 24 to 48 hours.
And since most of our minerals are consumed through food, reducing food intake drastically or completely fasting limits mineral intake.
Some of the most common signs of a potassium deficiency include:
- Constipation
- Heart palpitations
- Fatigue
- Muscle weakness
- Muscle twitches or spasms
- Numbness or tingling
- Muscle stiffness
To prevent the symptoms of electrolyte imbalance or hypokalemia, supplementation through a fast is recommended—and it won’t break your fast!
Here are some guidelines:
- Short fasts (24-48 hours) and IF/OMAD: Could benefit from electrolyte supplementation but not essential. This may depend on the status of the individual, activity level, and what you ate before starting your fast
- Extended fasts (over 48 hours): Use full electrolyte supplementation, especially if engaging in physical activity.
Some experts suggest that sodium, chloride, potassium, and magnesium are required for optimal fasting experience, but there’s minimal research available to support this.
That said, it’s never a bad idea and won’t cause harm if you do.
How To Determine The Optimal Level Of Fasting Electrolytes
Not sure whether you need more or less electrolytes during your fast?
There is no one-size-fits-all answer for finding the exact amount, but it becomes easy to tell once you get a feel for it after a couple of days of fasting.
Here are some signs to look out for on both ends of the spectrum:
Not enough electrolytes
- Headache
- Fatigue
- Dizziness
- Brain fog
- Nausea
- Muscle cramps or weakness
- Irregular or fast heartbeat
- Depression
Too many electrolytes
- Diarrhea
- Abdominal pain
- Nausea
- Swollen ankles and fingers
- Bloating
Where To Find Potassium

With all of that said, how do you get enough potassium?
If you need to supplement while fasting, you can choose a pure potassium supplement like Performance Lab Potassium, an electrolyte blend, or a multivitamin like Performance Lab NutriGenesis Multi—but in any case, it should supply enough to maintain levels and restore what was lost during a fast.

If you’re not fasting, ensure you consume potassium-rich foods to boost your levels. Some of the best options include:
- Cantaloupe
- Dried apricots
- Bananas
- Oranges
- Spinach
- Brussel sprouts
- Lentils
- Winter squash
- Beet greens
- Avocado
But what is the best solution? Do both!
Supplement during fasting and load up on potassium-rich foods when you’re not.
Related Post: Does Prebiotic Fiber Break a Fast? - A Complete Guide
References
- Weaver CM. Potassium and health. Adv Nutr. 2013;4(3):368S-77S.
- Terry J. The major electrolytes: sodium, potassium, and chloride. J Intraven Nurs. 1994;17(5):240-247.
- The principles of nerve cell communication. Alcohol Health Res World. 1997;21(2):107-108.
- Sweeney HL, Hammers DW. Muscle Contraction. Cold Spring Harb Perspect Biol. 2018;10(2):a023200.
- Brenner B, Eisenberg E. The mechanism of muscle contraction. Biochemical, mechanical, and structural approaches to elucidate cross-bridge action in muscle. Basic Res Cardiol. 1987;82 Suppl 2:3-16.
- Potter JD, Robertson SP, Johnson JD. Magnesium and the regulation of muscle contraction. Fed Proc. 1981;40(12):2653-2656.
- Daniels MC, Popkin BM. Impact of water intake on energy intake and weight status: a systematic review. Nutr Rev. 2010;68(9):505-521.
- Campbell I. Physiology of fluid balance. Anaesth Intensive Care Med. 2003;4(10):342-345.
- Hamm LL, Nakhoul N, Hering-Smith KS. Acid-Base Homeostasis. Clin J Am Soc Nephrol. 2015;10(12):2232-2242.
- Weinsier RL. Fasting--a review with emphasis on the electrolytes. Am J Med. 1971;50(2):233-240.