In 2019, about 528 million people lived with osteoarthritis - just one of many forms of joint pain. [1]
When you account joint pain from other sources, including injuries, inflammatory arthritis types, lupus, and other chronic diseases, this number is likely far greater.
It's therefore no surprise that many are asking: "what is the best joint pain treatment?"
This post cuts through the noise and gives you straightforward, evidence-backed answers to what works. Both short-term and long-term.
We'll cover therapies, exercise, natural remedies, supplements, surgery, and more; starting with a summary of key points right now.
Key Takeaways
-
Fast relief options. Nonsteroidal anti-inflammatory drugs and topical treatments like capsaicin cream can reduce pain quickly in the affected area, and many are available without a prescription. But they don't address root causes of chronic pain. [2, 3]
-
Movement for pain-free joints. Regular exercise helps strengthen muscles, maintain good posture, and directly supports cartilage health. Easing pain over time, not worsening it. [4]
-
Your diet directly impacts joint inflammation. A diet rich in anti-inflammatory foods (like fatty fish, leafy greens, and tart cherries) helps calm arthritis symptoms, while processed foods fuel them. Losing weight and keeping healthy weight is one of the key tips for knee pain. [5, 6]
-
Top supplements for joints include Boswellia Serrata, curcumin, type-II collagen, Omega-3s, and MSM. Each works differently and may help to ease pain and support cartilage. That said, scientific evidence for joint supplements is mixed, and they don't work for everyone. Expect to wait 4+ weeks to notice improvement with most nutritional supplements. Always go for third-party tested, reputable options. [7, 8]
-
Work with a physical or occupational therapist for personalized exercise plans. They'll teach you proper form and techniques to relieve stress on joints without causing further damage.
-
Advanced options when basics aren't enough. Injections (PRP, hyaluronic acid) can provide months of relief. An artificial joint may be necessary only when severe pain limits basic daily functions despite trying everything else. [9]
-
Sudden joint pain with fever is a red flag. If you get sudden joint pain with other symptoms like fever, chills, joint deformity, or inability to bear weight, call your doctor immediately. It could signal an infection.
-
Ease pain messages naturally by addressing inflammation at its source. Combine anti-inflammatory eating, targeted supplements, smart exercise, weight management, and professional advice for lasting results.
Why Joint Pain Happens & When to Worry

Joint pain can be inflammatory and non-inflammatory. [10, 11]
Inflammatory joint pain often comes "in a package" with other symptoms like swelling, tenderness, and stiffness after inactivity (e.g. after waking up in the morning). Causes include rheumatoid arthritis, psoriatic arthritis, lupus, or gout, among others.
Inflammatory joint pain is often systemic. The immune system doesn't work as it should, attacking healthy tissues, including joints. This means you can also feel other symptoms like fatigue or poor appetite, because inflammation affects other parts of your body.
Physical activity can reduce symptoms of inflammatory joint pain.
- Inflammatory joint pain can also be local, due to an injury. Your body sends inflammatory chemicals to an injured joint to deliver more blood and nutrients, thus promoting healing.
Non-inflammatory joint pain usually doesn't come with swelling or other symptoms from above. Fibromyalgia is one such example. [12, 13]
Osteoarthritis is another one. While it's often considered to be a non-inflammatory arthritis, more recent evidence suggests that inflammation hides behind osteoarthritis, too. [14, 15, 16]
It's a condition where cartilage - spongy tissue cushioning your joints - wears down. This results in increased friction between joints, ultimately leading to pain and joint damage.
Once you know your type of joint pain and its cause, it gets easier to narrow down the best treatment plans.
Can Joint Pain Resolve on Its Own?

In mild cases, after injury or overuse, joint pain can indeed resolve on its own. In these cases, rest and home care are often enough. But if you notice stubborn or worsening pain, it's time to call your doctor.
The answer to how long until joint pain goes away depends on the cause, severity, and how you treat it. A mild sprain might take up to two weeks to heal. [17] Inflammatory arthritis generally doesn't go away on its own and needs to be managed.
Fast Relief Strategies
The following quick relief strategies can be helpful when dealing with transient joint pain (e.g. from a mild injury).
These relief strategies include:
- NSAIDs and analgesics - highly effective for mild and moderate pain relief. They aren't meant for long-term use due to the risk of side effects for your liver, kidneys, heart, and other organs. [2]
- Topical creams - These include topical NSAIDs, natural gels, Voltaren, and other creams that offer fast and effective local relief. [3, 18]
- Hot and cold therapy - Ice packs for the first several hours after an injury, and heating pads or warm compress afterwards to aid blood flow and healing. [19, 20]
These are not a long-term solution, and don't address the root causes of joint pain. But they help to relieve symptoms, which makes the healing process more bearable.
Natural & Nutritional Support: How Your Gut Affects Your Joints

Foods can either promote or relieve inflammation.
What you eat affects your gut, where most of your immune system is. [21]
A diet based on ultra-processed foods and simple sugar is harmful to our gut, helping bad microbes to flourish and opens the door to inflammation. Including in your joints. [22]
Nutrients for Healthy Joints
Your body needs certain nutrients for optimal joint health and function.
For example, vitamin D plays a key role in modulating inflammation and keeping bones strong. [23] Low levels, which affect about a billion people worldwide, are linked to joint pain and fragile bones. [24] Getting more sun and eating fatty fish are the best ways to get enough vitamin D. [25]
Granted, many of us don't have access to direct sunlight that is strong enough to produce optimal vitamin D levels for most of the year. And some of us don't eat fish.
That leaves us with vitamin D supplements. Provided they are of high-quality, vitamin D supplements are a study-backed way to support optimal levels of this nutrient. [26]
Magnesium is another one - a mineral vital for bone and joint health. Just like with vitamin D, a big part of the world's population is not getting enough. [29] Magnesium helps regulate inflammation, contributes to a robust immune system, ensures healthy bone density and development, supports cartilage health and creation of new cells (chondrocytes). [27]
On the other hand, low magnesium is linked to inflammation and worsening of osteoarthritis.
Magnesium is found in dark leafy greens (kale), dark chocolate, avocado, whole grains, and different nuts and seeds. A high-quality magnesium supplement can make it easier to meet the daily value of 310-420 mg. [28]
Best Joint Pain Supplements
While vitamin D and magnesium form your nutritional foundation, certain herbs, spices, and specialized nutraceuticals may provide additional joint support when taken in supplemental doses.
A brief caveat: while some joint supplements are supported by studies, most of them need more robust human evidence to prove they really work and can benefit specific joint health parameters.
Additionally, supplements are not regulated the same way as medications. There is a lot of junk out there. Always choose third-party tested, reputable supplement brands.
With that in mind, here are some popular options that may help with joint discomfort:
Boswellia Serrata - for Pain and Inflammation
Boswellia Serrata, also known as Indian Frankincense, is a tree native to India, containing one of the best natural remedies for joint pain and inflammation.
Its resin contains potent Boswellic acids, particularly 3-O-acetyl-11-keto-beta-boswellic acid (AKBA), which has been studied for its potential to calm joint pain and stiffness.
One of the major systematic reviews of Boswellia in osteoarthritis recommends taking it for at least 4 weeks to see results. [30]
That said, Boswellia can work faster for some people than for others. A recent study of its effects on physical recovery in active men found benefits in reducing inflammation within 10 days of supplementation. [31]
Type-II Collagen - for Joint Strength and Daily Comfort
Type-II collagen is a protein that makes up about 90% of collagen in your cartilage. [32] Collagen holds your joints (and other tissues) together. In other words, our joints would fall apart without collagen to glue them.
Between the age of 25-30, your collagen levels start to decline. After 40, they may start to go down by 1% each year. [33]
Not only does the quantity of our collagen reduce, but so does the quality. This seems to contribute to cartilage loss and joint pain over time. [34]
There are ways you can combat this. Collagen supplements are shown to relieve pain and enhance joint comfort. [35] You'll often see two types of type-II collagen in supplement stores: undenatured and denatured (hydrolyzed) type-II collagen.
-
The undenatured collagen is essentially unprocessed collagen. It can potentially ease joint inflammation in rheumatoid arthritis and other autoimmune conditions that affect joints.
-
It appears to do this by training the immune system to stop attacking its own collagen structure in joints. Undenatured type-II collagen is often supplemented in very small doses, as low as 40 mg per day.
-
-
On the other hand, denatured or hydrolyzed type-II collagen is a more processed type of collagen.
-
It's exposed to heat, acid, and other factors that break down its triple helix structure, resulting in collagen peptides that are easier for your body to absorb.
-
As such, if you see supplements called "collagen peptides" and "hydrolyzed collagen", both are one and the same.
When you supplement hydrolyzed collagen, your body uses these broken-down peptides to make its own collagen, including in joints for cartilage.
Much like undenatured type-II collagen, the hydrolyzed counterpart is suggested to ease joint pain and inflammation in studies, but the supplemental dose is much higher; up to 10 g per day.
Glucosamine and Chondroitin - for General Joint Support
Glucosamine and chondroitin are components of your cartilage, playing a structural role and help provide resistance to compression, among others. [36]
They are some of the most popular joint supplements in the world. In some countries, they are classified as drugs.
They can be supplemented individually, but are more often taken together.
Studies show positive results but are inconclusive. Some research suggests that glucosamine and chondroitin (alone and in combination) may relieve knee pain and stiffness in certain contexts. [37, 38]
Although evidence is not yet clear on how good these supplements really are, many people report benefits in terms of joint pain.
Due to their popularity and safety for healthy people when taken in recommended doses, glucosamine and chondroitin might be worth trying if you struggle with joint pain.
MSM - for Cartilage, Lubrication Support, and Anti-Inflammatory Properties
MSM is an organic sulfur found in your body, plants, animals, and in everyday foods. It's essential for keeping your joints (and other body parts) healthy.
Taking MSM in the form of a supplement in doses higher than what's usually obtainable from food is suggested to help with joint pain. Though how effective it is, research still isn't clear.
It appears to work by calming the inflammation-amplifying NF-kB pathway. MSM also plays a role in cartilage protection and repair. [39]
This being said, MSM needs human studies to prove it works and under what conditions. While a quick internet search will show many positive testimonials, not everyone who takes MSM for joint pain sees results.
Turmeric (Curcumin) - for inflammation, pain & stiffness
Turmeric is considered by many to be an Indian superfood, or better said, a super-spice.
Thousands of years of traditional use as both food and medicine, coupled with the more recent evidence of its promising effects on health (including our joints), show it might actually live up to the reputation. [40, 41]
Turmeric's reason for popularity is mainly due to curcumin, its active compound. Curcumin is what gives turmeric its golden color and is believed to be behind many of the potential benefits — joint pain relief included.
Curcumin is one of the strongest natural anti-inflammatories that we currently know, with a systematic review from 2021 stating: "based on a small number of studies the effects are similar to that of NSAIDs." [40]
Another systematic review, while also recognizing the potential of turmeric for joint support, points to a need for more studies to draw any firm conclusions on turmeric's role in arthritis. [42]
On the anecdotal side of things, many people swear by curcumin for joint pain.
If you haven't already given it a chance, now is a time to consider, provided you're not taking medications that can it interact with, don't have health conditions, and have your doctor's approval (this applies to any supplement!).
You also need to make sure to take turmeric the right way, otherwise you may be wasting time and money.
The poor absorption of curcumin in the gut can be improved by approx. 2000% when you take turmeric with black pepper extract. If you want an easy way of achieving this, simply get a quality turmeric (or curcumin) supplement which contains black pepper extract.
Omega-3s - for lubrication, inflammation, and general joint support
Omega-3s are essential fatty acids stored in cell membranes all throughout your body, and most concentrated in your eyes, heart, and brain.
They support joint health by reducing inflammation, helping to lubricate joints, and easing discomfort and stiffness in osteoarthritis and other painful joint conditions.
Unlike omega-6, which are found in high amounts in the modern American diet, omega-3s are anti-inflammatory.
The ideal ratio of omega-6s to omega-3s is considered to be 4:1. Unfortunately, the modern Western diet is closer to 50:1 in favor of omega-6s, which is thought to contribute to a rise in many inflammatory conditions, including joint pain. [43, 44]
Our bodies don't produce omega-3s, so we need to get them through our diet.
Foods like fatty fish (sardines, salmon, trout) and chia seeds are good sources of omega-3s, but most people don't consume nowhere near enough. An effective alternative is taking a high-quality omega-3 supplement, whether from fish or algae, to enhance your blood levels of this joint-friendly fatty acid.
For a clean, third-party tested, algae-sourced omega-3 supplement, see Performance Lab® Omega-3.
Ginger - for pain and inflammation
Ginger is a flowering plant and spice related to turmeric, with anti-inflammatory properties of its own. Gingerols, the plant's active compounds, are shown to inhibit molecules in your body connected to pain signals. [45, 46]
Research hints that ginger may help with joint comfort and function in osteoarthritis. But some studies found no benefits for joint pain, at all. [47]
While evidence is inconclusive, we've deemed ginger worthy to make the list due to its safety, wide availability, and supportive benefits that may have a knock-on effect on joints.
What Supplement is The Most Powerful Anti-Inflammatory?

With so many options above, you might be wondering which supplements show the strongest evidence for joint pain relief.
- The ones showing the most promise for joint pain and inflammation relief include curcumin and Boswellia Serrata.
Best Indian herbs for joint pain include turmeric, ashwagandha, and possibly ginger. These are time-tested options that help to modulate inflammation naturally.
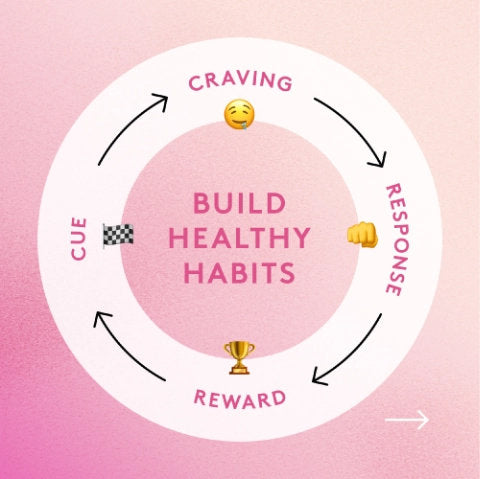
- Your consistency matters more than the dose alone. It can take four to eight weeks of steady use to show improvement.
The best way to go about it is to combine multiple supplements — to target pain and its underlying causes from different angles.
You can start by stacking some of the supplements from the list above.
Or if you want a more straightforward way, check Performance Lab® Flex, a third-party tested formula combining some of the ingredients from above in patented forms and low, daily dosages.
Test any supplement for 30 days and monitor symptoms. Ideally, on the day one of testing, write down a list of your symptoms and when they seem to be the worst. You can rate their severity from 1-10. Then, after 30 days of supplementation, write down the new numbers and see if, and how much your painful joints have improved.
Exercise, Physical Therapy & Movement

Movement is medicine for your joints. Regular exercise increases muscle strength and posture, lessening joint stress.
Not only that, but exercise may have a direct positive effect on joint inflammation and cartilage health — helping in osteoarthritis and other types of joint pain. [49]
Exercise also aids blood circulation and delivery of nutrients to joint tissue. This supports repair, maintenance, and lubrication.
Best exercises for joint pain include cycling, swimming, stretching, and strength training. However, what's best for someone might not be best for you; a rule of thumb is to avoid exercises that worsen your pain.
If you're inexperienced, consider getting a personal trainer, especially with strength training. They can help you learn the foundations for building strong supporting muscles to correct gait and posture.
A physical therapist can help you learn specialized exercises to improve joint comfort, mobility, and function. They may teach you how to best use hot and cold compress for quick pain relief, give advice to reduce the risk of injuries, or recommend wearing braces and splints for joint support and shoe inserts to ease leg stress.
Quickest Exercises for Joint Pain Relief
Static stretches are effective for increasing joint range of motion (ROM) and flexibility. Stretching also appears to soothe musculoskeletal pain. [48]
Hold each stretch for 30-60 seconds, rest in between each set, and do this with every achy part of the body.
Strength training, done with proper posture and form, can strengthen shock absorption of your legs when walking.
Different types of exercise, including isometric and isotonic exercises like lunges, squats, planks, and dumbbell curls, are shown to ease joint pain and stiffness. [49]
Never use heavy weights if inexperienced to not worsen pain or cause an injury. Start with body weight exercises and progress gradually from there.
Remember that more isn't always better. Animal research suggests excessive, hard training can negatively affect joints. [50]
Here's a simple start: walk daily, stretch major joints, and keep workouts short but regular. Your pain should ease with repetition, not worsen!
Fasting and Joint Pain Relief: Does it Work?

Fasting has become an increasingly popular tool for all things health. But what about joints?
According to limited research, abstaining from food and other sources of calories for 16+ hours may assist in relieving pain in some contexts, such as in people with osteoarthritis. It may help in both the short-term and long-term. [51]
- Short-term, by reducing pro-inflammatory molecules that spark joint pain.
- Long-term, by assisting weight loss and reducing pressure on your joints.
That said, not all studies found benefits with fasting for joint pain. For example, a study with obese postmenopausal women with rheumatoid arthritis found a reduction in body mass index, but didn't notice significant reductions in inflammation and other markers of rheumatoid arthritis.
Strong evidence supporting fasting for joint pain is scarce, and for some people, fasting can cause negative side effects instead of positive changes. [52]
Still, a mix of lab and human research shows fasting does have a potential to ease pain and support other aspects of joint health.
A 2016 cell study found that insulin can negatively affect joint cartilage and elevate inflammatory markers. Authors of the study proposed that decreasing fasting insulin levels might play a role in reducing inflammation and cartilage damage (both of which can make joints hurt). [53] Fasting is well-known for helping reduce insulin and promote insulin sensitivity.
Another 2017 clinical trial with 37 OA patients found that fasting can significantly reduce joint pain and improve physical function and quality of life. What's more, they found that these benefits lasted even after the patients stopped fasting. [54]
While it may not work for everyone, if you're healthy and have an approval from your doctor, fasting might be worth trying to support comfortable joints.
Injections, Regenerative Therapies & Advanced Options

For some people, physical therapy, supplements, and dietary changes aren't enough to relieve pain.
In these cases, your doctor may suggest more advanced therapies like hyaluronic acid injections, stem cell therapy, PRP, or steroid injections.
Each of these has its pros and cons. [56]
- Steroid injections - also known as cortisone injections or steroid shots, this is a go-to injection treatment for arthritis. Cortisone injections mimic natural cortisol to reduce inflammation and pain. This also makes them helpful for transient causes of joint pain, such as injuries. However, they can only be taken a few times per year, and come with a risk of side effects like heightened blood sugar levels and adrenal problems. [55]
- Hyaluronic acid visco-supplementation - Hyaluronic acid is a natural lubricant in your joints. A healthcare provider injects hyaluronic acid into a painful joint, which helps with lubrication and can ease inflammation and pain. [59]
- PRP - Platelet-rich plasma injections contain concentrated components of your own blood (platelets and plasma). A doctor injects these into the joint to promote faster healing and pain relief. PRP is considered safer than steroid injections and possibly more effective than hyaluronic acid injections (but also more expensive). [58]
- Stem cell therapy - stem cells are undesigned cells that can morph into different types of cells, including those that make up your joints. Early research suggests that stem cell injections may help relieve pain to some extent. However, studies are inconclusive - we need more research to determine how helpful stem cell therapy really is for joint pain. [55]
Joint Replacement Surgery & When It’s Justified

Hip and knee replacements are the two most common joint replacement surgeries. [60] Other common procedures include osteotomy (part of a bone is cut and repositioned or reshaped to relieve joint pressure) and arthroscopy (doctor uses a specialized device to look inside a joint and treat issues).
Surgery is often the last resort. It may be necessary if your pain is disabling despite trying all the above non-surgical options.
Keep in mind that joint replacement surgeries are expensive, take a long time to fully heal, risk deep wound infections and nerve injuries, and may be followed with more surgeries in the future as implants wear down and need replacement.
How bad must the knee or another joint be to need surgery? It's when the pain or joint damage is so severe that it limits your basic daily functions.
Long-Term Relief & Maintenance Strategy

Long-term relief from joint pain starts with uncovering the cause.
Joint pain that comes from an injury will often heal on its own with proper care and rest. On the other hand, osteoarthritis and inflammatory arthritis calls for deeper lifestyle changes such as:
- Following an anti-inflammatory diet (like a Mediterranean diet).
- Regular exercise, including strength training for joint-supporting muscles.
- Hot and cold therapy for flares, and, when absolutely necessary, OTC painkillers.
- Consistent use of joint-specialized formulas such as Performance Lab® Flex and Omega-3 for an additional layer of support for your joints.
- Weight management and regular fasting, as every extra pound adds several pounds of pressure on your knees and hips.
- Physical therapy once a month to learn proper posture exercises to relieve pain and joint stress.
- Getting 7-9 hours of sleep per night to support recovery and modulate inflammation.
Joint Pain FAQs
- What is the most effective treatment for knee pain? - Pain-relieving medications such as NSAIDs tend to offer the fastest relief from knee pain. Cortisone injections or PRP therapy are also effective treatments, but are more complicated and don't work immediately. For natural support, a combination of regular movement, anti-inflammatory nutrition, and targeted supplements supported by physical therapy offers consistent results.
- What vitamin deficiency causes joint pain? - Vitamin D and magnesium are common deficiencies that can worsen inflammation and stiffness.
- What is the best medicine or tablet for joint pain & arthritis? There is no single best medicine or tablet for arthritis and joint pain. For many people, OTC painkillers can successfully treat mild to moderate pain. Natural options include Boswellia Serrata, curcumin, MSM, and glucosamine.
- Is there any cure for joint pain? Many people recover fully from joint pain, especially from injuries or inflammation. With arthritis, lasting relief is absolutely possible with the right approach. The path to complete healing varies from person to person.
- How to permanently get rid of joint pain? - You can stop progression of joint pain and restore comfort through physical therapy, an anti-inflammatory diet, specialized supplements, and joint injections.
- What is the best topical cream or joint gel? - Popular and effective options for localized pain include Voltaren, NSAID creams like dicoflenac gel, and menthol creams.
- Do stem cells work? - Stem cell therapy isn't a definitive answer to joint pain. Emerging studies show promising results, but it's still inconclusive.
- How long until joint pain goes away? - Joint pain can take several days to several weeks to heal from a minor sprain or injury, whereas chronic arthritis pain can persist, often coming and going.
Final Thoughts
There is no one-size-fits-all joint pain treatment.
The best treatment may use several levers like nutrition overhaul, following a joint-friendly exercise program, and smart supplementation targeting specific joint issues.
For more severe cases limiting daily life, injections, professional therapy, or surgery may be needed.
Start with the basics from above, and consider adding a high-quality supplement like Performance Lab® Flex. It's designed to complement your joint health routine and promote comfortable movement.

Flex uses AprèsFlex® Boswellia serrata and CurcuWIN® curcumin, as well as a blend of Phytodroitin™, OptiMSM® and corn glucosamine — with low ingredient dosages for safe daily use.
References
- World Health Organization. (2023, July 14). Osteoarthritis. https://www.who.int/news-room/fact-sheets/detail/osteoarthritis
- Hopkins, S., Yang, V., & Liew, D. F. (2025). Choosing a nonsteroidal anti-inflammatory drug for pain. Australian prescriber, 48(4), 139–144. https://doi.org/10.18773/austprescr.2025.032
- Tshering, G., Posadzki, P., & Kongkaew, C. (2024). Efficacy and safety of topical capsaicin in the treatment of osteoarthritis pain: A systematic review and meta-analysis. Phytotherapy research : PTR, 38(7), 3695–3705. https://doi.org/10.1002/ptr.8223
- Zeng, C. Y., Zhang, Z. R., Tang, Z. M., & Hua, F. Z. (2021). Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Frontiers in physiology, 12, 794062. https://pmc.ncbi.nlm.nih.gov/articles/PMC8716769/
- Yu, X., Pu, H., & Voss, M. (2024). Overview of anti-inflammatory diets and their promising effects on non-communicable diseases. The British journal of nutrition, 132(7), 898–918. https://doi.org/10.1017/S0007114524001405
- Ciaffi, J., Mancarella, L., Ripamonti, C., D'Amuri, A., Brusi, V., Pignatti, F., Lisi, L., & Ursini, F. (2025). Ultra-Processed Food and Its Impact on Bone Health and Joint Diseases: A Scoping Review. Nutrients, 17(7), 1188. https://doi.org/10.3390/nu17071188
- Colletti, A., & Cicero, A. F. G. (2021). Nutraceutical Approach to Chronic Osteoarthritis: From Molecular Research to Clinical Evidence. International journal of molecular sciences, 22(23), 12920. https://doi.org/10.3390/ijms222312920
- Liu, X., Machado, G. C., Eyles, J. P., Ravi, V., & Hunter, D. J. (2018). Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. British journal of sports medicine, 52(3), 167–175. https://doi.org/10.1136/bjsports-2016-097333
- Qiao, X., Yan, L., Feng, Y., Li, X., Zhang, K., Lv, Z., Xu, C., Zhao, S., Liu, F., Yang, X., & Tian, Z. (2023). Efficacy and safety of corticosteroids, hyaluronic acid, and PRP and combination therapy for knee osteoarthritis: a systematic review and network meta-analysis. BMC musculoskeletal disorders, 24(1), 926. https://doi.org/10.1186/s12891-023-06925-6
- Akhondi, H., Blum, M. A., & Gupta, N. (2025, August 9). Polyarticular arthritis. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK537170/
- Poudel, P., & Lappin, S. L. (2023). Inflammatory Arthritis. In StatPearls. StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/29939526/#:~:text=Excerpt,to%20joint%20damage%20and%20deformities.
- American College of Rheumatology. (2025, February). Fibromyalgia. Retrieved from https://rheumatology.org/patients/fibromyalgia
- Siracusa, R., Paola, R. D., Cuzzocrea, S., & Impellizzeri, D. (2021). Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. International journal of molecular sciences, 22(8), 3891. https://doi.org/10.3390/ijms22083891
- Knights, A. J., Redding, S. J., & Maerz, T. (2023). Inflammation in osteoarthritis: the latest progress and ongoing challenges. Current opinion in rheumatology, 35(2), 128–134. https://doi.org/10.1097/BOR.0000000000000923
- de Rezende, M. U., & de Campos, G. C. (2013). Is osteoarthritis a mechanical or inflammatory disease?. Revista brasileira de ortopedia, 48(6), 471–474. https://doi.org/10.1016/j.rboe.2013.12.002
- Sen, R., & Hurley, J. A. (2023, February 20). Osteoarthritis. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482326/
- Bergman, R., & Shuman, V. L. (2025, August 2). Acute ankle sprain. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459212/
- Wang, Y., Fan, M., Wang, H., You, Y., Wei, C., Liu, M., Luo, A., Xu, X., & Duan, X. (2022). Relative safety and efficacy of topical and oral NSAIDs in the treatment of osteoarthritis: A systematic review and meta-analysis. Medicine, 101(36), e30354. https://doi.org/10.1097/MD.0000000000030354
- Brosseau, L., Yonge, K. A., Robinson, V., Marchand, S., Judd, M., Wells, G., & Tugwell, P. (2003). Thermotherapy for treatment of osteoarthritis. The Cochrane database of systematic reviews, 2003(4), CD004522. https://doi.org/10.1002/14651858.CD004522
- Rossi R. (2024). Heat therapy for different knee diseases: expert opinion. Frontiers in rehabilitation sciences, 5, 1390416. https://pmc.ncbi.nlm.nih.gov/articles/PMC11270809/#s7
- Zhang P. (2022). Influence of Foods and Nutrition on the Gut Microbiome and Implications for Intestinal Health. International journal of molecular sciences, 23(17), 9588. https://doi.org/10.3390/ijms23179588
- Longo, U. G., Lalli, A., Bandini, B., de Sire, R., Angeletti, S., Lustig, S., Ammendolia, A., Budhiparama, N. C., & de Sire, A. (2024). Role of the Gut Microbiota in Osteoarthritis, Rheumatoid Arthritis, and Spondylarthritis: An Update on the Gut-Joint Axis. International journal of molecular sciences, 25(6), 3242. https://doi.org/10.3390/ijms25063242
- Laird, E., Ward, M., McSorley, E., Strain, J. J., & Wallace, J. (2010). Vitamin D and bone health: potential mechanisms. Nutrients, 2(7), 693–724. https://doi.org/10.3390/nu2070693
- Palacios, C., & Gonzalez, L. (2014). Is vitamin D deficiency a major global public health problem?. The Journal of steroid biochemistry and molecular biology, 144 Pt A, 138–145. https://doi.org/10.1016/j.jsbmb.2013.11.003
- Nagaria, T. D., Shinde, R. K., Shukla, S., Acharya, S., Acharya, N., & Jogdand, S. D. (2023). The Sunlight-Vitamin D Connection: Implications for Patient Outcomes in the Surgical Intensive Care Unit. Cureus, 15(10), e46819. https://doi.org/10.7759/cureus.46819
- Pludowski, P., Grant, W. B., Karras, S. N., Zittermann, A., & Pilz, S. (2024). Vitamin D Supplementation: A Review of the Evidence Arguing for a Daily Dose of 2000 International Units (50 µg) of Vitamin D for Adults in the General Population. Nutrients, 16(3), 391. https://doi.org/10.3390/nu16030391
- Li, G., Cheng, T., & Yu, X. (2021, December 23). The impact of trace elements on osteoarthritis. Frontiers in Medicine, 8, 771297. https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.771297/full
- U.S. Food & Drug Administration. (2024, March 5). Daily Value on the Nutrition and Supplement Facts Labels.
- DiNicolantonio, J. J., O'Keefe, J. H., & Wilson, W. (2018). Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open heart, 5(1), e000668. https://doi.org/10.1136/openhrt-2017-000668
- Yu, G., Xiang, W., Zhang, T., Zeng, L., Yang, K., & Li, J. (2020). Effectiveness of Boswellia and Boswellia extract for osteoarthritis patients: a systematic review and meta-analysis. BMC complementary medicine and therapies, 20(1), 225. https://pmc.ncbi.nlm.nih.gov/articles/PMC7368679/
- Salter, D., Yalamanchi, H., Yalamanchi, A., & Yalamanchi, A. (2025). Ten days of supplementation with a standardized Boswellia serrata extract attenuates soreness and accelerates recovery after repeated bouts of downhill running in recreationally active men. Frontiers in sports and active living, 7, 1488821. https://pmc.ncbi.nlm.nih.gov/articles/PMC11798962/
- Sophia Fox, A. J., Bedi, A., & Rodeo, S. A. (2009). The basic science of articular cartilage: structure, composition, and function. Sports health, 1(6), 461–468. https://doi.org/10.1177/1941738109350438
- Arthritis Foundation. (n.d.). Can collagen supplements help arthritis? Retrieved from https://www.arthritis.org/health-wellness/treatment/complementary-therapies/supplements-and-vitamins/can-collagen-supplements-help-arthritis
- Ouyang, Z., Dong, L., Yao, F., Wang, K., Chen, Y., Li, S., Zhou, R., Zhao, Y., & Hu, W. (2023). Cartilage-Related Collagens in Osteoarthritis and Rheumatoid Arthritis: From Pathogenesis to Therapeutics. International journal of molecular sciences, 24(12), 9841. https://doi.org/10.3390/ijms24129841
- Martínez-Puig, D., Costa-Larrión, E., Rubio-Rodríguez, N., & Gálvez-Martín, P. (2023). Collagen Supplementation for Joint Health: The Link between Composition and Scientific Knowledge. Nutrients, 15(6), 1332. https://doi.org/10.3390/nu15061332
- National Center for Complementary and Integrative Health. (2023, October). Glucosamine and chondroitin for osteoarthritis: What you need to know. https://www.nccih.nih.gov/health/glucosamine-and-chondroitin-for-osteoarthritis-what-you-need-to-know
- Baden, K. E. R., Hoeksema, S. L., Gibson, N., Gadi, D. N., Craig, E., Draime, J. A., Tubb, S. M., & Chen, A. M. H. (2025). The Safety and Efficacy of Glucosamine and/or Chondroitin in Humans: A Systematic Review. Nutrients, 17(13), 2093. https://doi.org/10.3390/nu17132093
- Fernández-Martín, S., González-Cantalapiedra, A., Muñoz, F., García-González, M., Permuy, M., & López-Peña, M. (2021). Glucosamine and Chondroitin Sulfate: Is There Any Scientific Evidence for Their Effectiveness as Disease-Modifying Drugs in Knee Osteoarthritis Preclinical Studies?-A Systematic Review from 2000 to 2021. Animals : an open access journal from MDPI, 11(6), 1608. https://doi.org/10.3390/ani11061608
- Toguchi, A., Noguchi, N., Kanno, T., & Yamada, A. (2023). Methylsulfonylmethane Improves Knee Quality of Life in Participants with Mild Knee Pain: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients, 15(13), 2995. https://doi.org/10.3390/nu15132995
- Paultre, K., Cade, W., Hernandez, D., Reynolds, J., Greif, D., & Best, T. M. (2021). Therapeutic effects of turmeric or curcumin extract on pain and function for individuals with knee osteoarthritis: a systematic review. BMJ open sport & exercise medicine, 7(1), e000935. https://doi.org/10.1136/bmjsem-2020-000935
- Hewlings, S. J., & Kalman, D. S. (2017). Curcumin: A Review of Its Effects on Human Health. Foods (Basel, Switzerland), 6(10), 92. https://doi.org/10.3390/foods6100092
- Daily, J. W., Yang, M., & Park, S. (2016). Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Journal of medicinal food, 19(8), 717–729. https://doi.org/10.1089/jmf.2016.3705
- Mariamenatu, A. H., & Abdu, E. M. (2021). Overconsumption of omega-6 polyunsaturated fatty acids (PUFAs) versus deficiency of omega-3 PUFAs in modern-day diets: The disturbing factor for their “balanced antagonistic metabolic functions” in the human body. Journal of Lipids, 2021, Article 8848161. https://doi.org/10.1155/2021/8848161
- DiNicolantonio, J. J., & O'Keefe, J. (2021). The Importance of Maintaining a Low Omega-6/Omega-3 Ratio for Reducing the Risk of Autoimmune Diseases, Asthma, and Allergies. Missouri medicine, 118(5), 453–459.
- Mao, Q. Q., Xu, X. Y., Cao, S. Y., Gan, R. Y., Corke, H., Beta, T., & Li, H. B. (2019). Bioactive Compounds and Bioactivities of Ginger (Zingiber officinale Roscoe). Foods (Basel, Switzerland), 8(6), 185. https://doi.org/10.3390/foods8060185
- Szymczak, J., Grygiel-Górniak, B., & Cielecka-Piontek, J. (2024). Zingiber Officinale Roscoe: The Antiarthritic Potential of a Popular Spice-Preclinical and Clinical Evidence. Nutrients, 16(5), 741. https://doi.org/10.3390/nu16050741
- Araya-Quintanilla, F., Gutierrez-Espinoza, H., Munoz-Yanez, M. J., Sanchez-Montoya, U., & Lopez-Jeldes, J. (2020). Effectiveness of Ginger on Pain and Function in Knee Osteoarthritis: A PRISMA Systematic Review and Meta-Analysis. Pain physician, 23(2), E151–E161. https://pubmed.ncbi.nlm.nih.gov/32214292/
- Konrad, A., Nakamura, M., Sardroodian, M., Aboozari, N., Anvar, S. H., & Behm, D. G. (2025). The effects of chronic stretch training on musculoskeletal pain. European journal of applied physiology, 125(8), 2037–2048. https://pmc.ncbi.nlm.nih.gov/articles/PMC12354564/
- Zeng, C. Y., Zhang, Z. R., Tang, Z. M., & Hua, F. Z. (2021). Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Frontiers in physiology, 12, 794062. https://pmc.ncbi.nlm.nih.gov/articles/PMC8716769/
- Wang, W., Niu, Y., & Jia, Q. (2022). Physical therapy as a promising treatment for osteoarthritis: A narrative review. Frontiers in physiology, 13, 1011407. https://pmc.ncbi.nlm.nih.gov/articles/PMC9614272/
- Sun, N., Zhao, Y., Wang, J., Zhang, A., & He, Y. (2025). Intermittent fasting in osteoarthritis: from mechanistic insights to therapeutic potential. Frontiers in nutrition, 12, 1604872. https://pmc.ncbi.nlm.nih.gov/articles/PMC12318773/#:~:text=Collectively%2C%20these%20findings%20indicate%20that,necessary%20to%20confirm%20these%20observations
- Ranjbar, M., Shab-Bidar, S., Rostamian, A., Mohammadi, H., Tavakoli, A., & Djafarian, K. (2025). Effects of intermittent fasting diet in overweight and obese postmenopausal women with rheumatoid arthritis: A randomized controlled clinical trial. Complementary therapies in medicine, 91, 103189. https://doi.org/10.1016/j.ctim.2025.103189
- Ribeiro, M., López de Figueroa, P., Blanco, F. J., Mendes, A. F., & Caramés, B. (2016). Insulin decreases autophagy and leads to cartilage degradation. Osteoarthritis and cartilage, 24(4), 731–739. https://doi.org/10.1016/j.joca.2015.10.017
- Drinda, S., Franke, S., Schmidt, S., Stoy, K., Lehmann, T., Wolf, G., & Neumann, T. (2018). AGE-RAGE interaction does not explain the clinical improvements after therapeutic fasting in osteoarthritis. Complementary Medicine Research, 25(3), 167–172. https://doi.org/10.1159/000486237
- Kamel, S. I., Rosas, H. G., & Gorbachova, T. (2024). Local and Systemic Side Effects of Corticosteroid Injections for Musculoskeletal Indications. AJR. American journal of roentgenology, 222(3), e2330458. https://doi.org/10.2214/AJR.23.30458
- Ayhan, E., Kesmezacar, H., & Akgun, I. (2014). Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World journal of orthopedics, 5(3), 351–361. https://pmc.ncbi.nlm.nih.gov/articles/PMC4095029/
- Whittle, S. L., Johnston, R. V., McDonald, S., Worthley, D., Campbell, T. M., Cyril, S., Bapna, T., Zhang, J., & Buchbinder, R. (2025). Stem cell injections for osteoarthritis of the knee. The Cochrane database of systematic reviews, 4(4), CD013342. https://doi.org/10.1002/14651858.CD013342.pub2
- Crowley, J. L., & Soti, V. (2023). Platelet-Rich Plasma Therapy: An Effective Approach for Managing Knee Osteoarthritis. Cureus, 15(12), e50774. https://doi.org/10.7759/cureus.50774
- Ranawat, A., Guo, K., Phillips, M., Guo, A., Niazi, F., Bhandari, M., & Waterman, B. (2024). Health Economic Assessments of Hyaluronic Acid Treatments for Knee Osteoarthritis: A Systematic Review. Advances in therapy, 41(1), 65–81. https://pubmed.ncbi.nlm.nih.gov/37899384/
- Seidlitz, C., & Kip, M. (2018). Introduction to the indications and procedures. In H. H. Bleß & M. Kip (Eds.), White paper on joint replacement: Status of hip and knee arthroplasty care in Germany (Chap. 1). Springer. https://www.ncbi.nlm.nih.gov/books/NBK546138/