Digestive discomfort, bloating, and unpredictable gut symptoms can quickly take over daily life, especially for people living with IBS or SIBO. The low fermentation diet has emerged as a practical, research-supported approach to easing these symptoms by reducing the foods most likely to feed excess bacteria in the small intestine.
In this guide, we break down exactly how the low fermentation diet works, why it may help relieve symptoms, and how it compares to similar approaches like the Low FODMAP diet.
This essential overview will help you understand what the diet involves, what you can eat, and what to consider before starting.
Key Takeaways
- The low-fermentation diet helps reduce bloating, gas, and discomfort by limiting foods that feed excess gut bacteria.
- It focuses on easy-to-digest carbs, lean proteins, and low-fibre fruits/vegetables while avoiding high-fibre, highly fermentable foods.
- Well-spaced meals support intestinal “clean-up” waves that reduce fermentation and digestive symptoms.
- Because the diet is restrictive and low in fibre, using a comprehensive multivitamin like Performance Lab® NutriGenesis® Multi can help support nutrient balance.

What is the Low Fermentation diet?
This is a restrictive eating plan that seeks to reduce fermentable carbohydrates in the diet by limiting high fibre foods, and is most often followed by people suffering with IBS or SIBO (details of these conditions below).
High fibre foods can feed the bacteria causing these debilitating conditions and avoiding these foods can reduce bacterial fermentation.
Cedars-Sinai Diet
You may also hear it called the Cedars-Sinai diet after first being developed by Dr. Mark Pimentel of Cedars-Sinai Hospital in Los Angeles, California.
Let's take a quick look at the conditions a low fermentation diet may be used to help:
Small Intestinal Bacterial Overgrowth (SIBO)

SIBO is a digestive disorder marked by an abnormal increase in the bacteria in the small intestines or small bowel. It may be caused by surgery or disease which slows the passage of food and waste through the digestive tract, creating a breeding ground for bacteria. This excess bacteria - often not normally found in the small intestine - may cause weight loss, malnutrition and diarrhea.
It is estimated that up to 40% of patients with IBS also have SIBO. Some researchers put that figure much higher. (1)
Irritable Bowel Syndrome (IBS)

This is the most common gastrointestinal disorder in the world, affecting 10-15% of the population. Two-thirds of those are women. Symptoms include changes in bowel habits such as diarrhea, constipation, plus severe cramping and bloating, and can be debilitating, interrupting everyday life.
While the low fermentation diet was originally designed with SIBO in mind, it may also prove helpful to people with IBS as well, especially given the potential crossover between the two for many people. (2)
Mild cases of the above may be managed with diet and nutrition - such as the low fermentation diet - as well as lifestyle and managing stress, while severe cases may need medicine.
All About Fermentation
Before we discuss the low fermentation diet in any detail, we should probably make sure we're aware of what fermentation means and why it can cause issues for people with IBS or SIBO patients.
Let's take it step by step:
-
Fermentation is what happens when microbes in the gut break down complex carbohydrates that are not easily digested by the body. (Read on for a list of such complex carbs to avoid)
-
The process creates beneficial SCFAS - short-chain fatty acids, important for gut health and the health of several other systems.
-
This process provides energy for cells lining the colon and can help to boost absorption of nutrients. So far, so good. Here's where the issues arise..
-
As a by-product, this process also generates gases such as methane, carbon dioxide and hydrogen which may cause bloating, abdominal pain and flatulence in some people.
-
For people with IBS and SIBO, this can be a more serious problem. It can be painful and can exacerbate damage to the lining of the gut. (3)
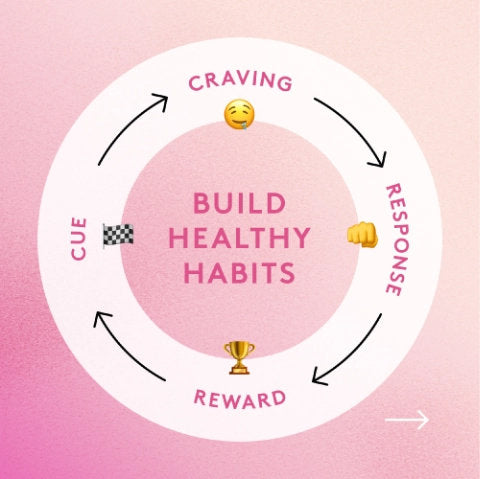
Key Principles of the Low Fermentation Diet
There are several key principles of the low fermentation diet. They include:
-
Reducing high dietary fiber foods such as wholewheat breads
-
Opting instead for easy-to-digest carbs such as rice, potatoes or white bread
-
Limit snacking
-
Spacing meals, making sure there's a 4-5 hour gap between meals and you eat at least two hours before bed.
-
Eating the same amount of food but as distinct meals rather than snacking to allow your gut time to empty.
The latter is important because of something called the Migrating Motor Complex (MMC). Consider this like a 'cleaning wave' or 'housekeeping wave' in your small intestine that takes place every 90-120 minutes or so, while you are in a fasted state. This wave or rhythmic contraction removes all leftover debris from food (as well as microbes) and sweeps them into the colon.
Eating on a regular basis doesn't allow this cleaning wave to occur. Careful meal spacing can ensure any excess bacteria in your small intestine has little to munch on, causing fewer symptoms. (4, 5)
How Does This Differ to the Low FODMAP Diet?

You may have also heard of a very similar diet called the Low FODMAP diet, another diet which is often recommended for people with IBS and SIBO.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, poorly absorbed carbohydrates (sugars) that can cause digestive upset, found within grains, dairy products, fruits, vegetables, and more.
The Low FODMAP diet tends to be stricter than the low fermentation diet, although it has many similarities. You are allowed to have garlic and onion on the low fermentation diet, for example, but not on the Low FODMAP diet. Portion sizes of certain foods may be smaller on the Low FODMAP diet.
The Low FODMAP diet is often described as an elimination diet and has three phases - you start by reducing foods or eliminating all of the high-FODMAP foods for 2-4 weeks before a reintroduction phase where you systematically add foods back to your diet.
A third maintenance phase is where you keep what works for you and scrap what doesn't. A food dairy may help you to discover any potential triggers for symptom management. (6, 7)
To Summarise: The Low Fermentation Diet...
The diet asks you to limit high fiber foods, avoid high FODMAP foods, and promote meal spacing.
Low Fermentation Foods: What Can You Eat on a Low Fermentation Diet?

Foods allowed on the low fermentation diet include:
-
Beef, chicken, eggs, fish, pork. Protein is important
-
Refined carbohydrates or easy to digest carbohydrates such as white bread and white rice.
-
Vegetables such as peppers, carrots, cucumbers, onions, garlic, yams, beets, turnips zucchini, tomatoes, egg plant, peas (avoid the pod), potatoes, mushrooms. Essentially, vegetables that grow under the ground or grow off a plant are ok on this diet.
-
Fruits are allowed, but avoid those high in fructose such as apples, pears, or mangos.
-
Opt for lactose free milk and dairy products low in lactose, such as hard cheeses for a rare treat.
-
Nuts and seeds.
-
Oils or healthy fats.
-
Sugars - sucrose (table sugar) and glucose are easier to absorb.
-
Drink 5-8 cups of water a day. (8)
TO SUMMARISE...
Typically well-tolerated foods include lean proteins, low fiber vegetables, and low FODMAP fruits like berries and citrus fruits.
What to Avoid on a Low Fermentation Diet (High FODMAP Foods)

-
Beans and legumes
-
Humus
-
Brussels sprouts, broccoli, cauliflower, cabbage, and leafy vegetables. (If you have a salad, make it a small side salad)
-
Apples, pears, ripe bananas and other high-fructose fruits.
-
Whole wheat or multigrain breads, and whole grains.
-
Gum, which often contains ferementable sugar alcohols such as sorbitol.
-
Dairy products such as cheese and yogurt, and non-lactaid milk - all contain lactose
-
Splenda
-
While chocolate is allowed, limit milk chocolate
-
Avoid products with added fiber, such as certain breakfast cereals
-
Avoid artificial sweeteners and hard to absorb sugars such as lactose (milk sugar) and fructose (in fruits), as well as Sucralose (Splenda™), Sorbitol (in sugar free gum) Xylitol, Lactulose, Lactitol etc...
-
Minimize sodas. Avoid ones in particular that include sucralose or Splenda. (8)
TO SUMMARISE...
Foods high in FODMAPs, such as wheat pasta, cruciferous vegetables, and certain fruits, should be limited or avoided. Processed meats and high fructose corn syrup should also be avoided due to their potential to exacerbate gastrointestinal symptoms.
Does a Low Fermentation Diet Work?
As I mentioned, the low fermentation diet has been recommended for IBS and SIBO sufferers in particular. But is there evidence that it helps to reduce uncomfortable symptoms?
Apparently so. As one clinical trial into IBS concluded:
"Although there is no evidence that a low-fermentation diet alone rebalances the microbiota of the small intestine or permanently reverses symptoms, it has been shown to significantly improve the patients’ symptoms over time. This diet relieves discomfort, abdominal distension, gas production, and diarrhea."
Such symptomatic relief can help patients halt the weight loss caused by chronic diarrhea and, more importantly, improve their mood, energy levels, and quality of life." (9)
Limitations of the Low Fermentation Diet
While all of this sounds hopeful for sufferers of IBS and SIBO, there are some limitations to be aware of. As touched on above, diet alone cannot be expected to reverse or cure these conditions.
Most experts believe this diet can be just one tool in your potential arsenal alongside antibiotics or other treatments or ways of managing SIBO or IBS.
Likewise, this is not intended to be a permanent way of eating. This is why...
Gut Microbiome Connection
By reducing the amount of fermentable carbohydrates you eat, you are essentially depriving the gut bacteria in your intestinal microbiome of food, which may reduce its diversity over time.
A diverse microbiota in your gastrointestinal tract offers significant health benefits over and above digestion, so damaging this may cause more problems than benefits. The reduced fiber may also worsen any constipation problems.
High Glycemic Index
Be aware too that this diet tends to have a higher glycemic index than a diet high in fiber (all that white bread!) This is an important factor for anyone with diabetes or prediabetes. (10)
Nutritional Gaps
Following these diet restrictions for a long period of time - anything over three months - may lead to damaging nutritional gaps or even malnourishment. (2)
Top Up Your Nutrients with a Quality Multivitamin
The restrictions of the low fermentation diet potentially puts dieters at risk for several key nutrients. A systematic review of 26 studies, for instance, determined that IBS patients and those on such exclusion diets had a low intake of B vitamins, vitamin D, calcium, iron, and zinc, all crucial nutrients. (11)
One way to support overall nutrient intake when temporarily following a restrictive diet is to take a quality multivitamin supplement, such as Performance Lab NutriGenesis Multi.
With special formulas for men and women, this multivitamin includes generous dosages of most of the above (potentially missing) nutrients, as well as many more. It provides the recommended daily intake of at least 15 vitamins and minerals.
Made using a proprietary technology called NutriGenesis, the vitamins and minerals included in this multivitamin are identical to the forms you'd find in nature, making them highly bioavailable and easier to absorb.
The only multi I’ve used and noticed more energy and better overall wellbeing!Jerrold N

Final Thoughts
Irritable bowel syndrome (IBS) and SIBO can be debilitating and impact on everyday life. Managing IBS symptoms is often challenging, and it's not surprising that sufferers are keen to investigate various strategies to gain a better understanding of their condition.
Studies have shown that elimination diets and low fermentation eating may potentially help alleviate symptoms of IBS and SIBO even if it doesn't necessarily address the primary cause or inflammation.
However, such a restrictive diet should only be a short term plan as it potentially interferes with beneficial bacteria in the gut and large intestine. It may also decrease the overall nutrient intake which a quality multivitamin like Performance Lab NutriGenesis Multi may help address.
Of course, gaining an official diagnosis first is important to ascertain what issues you have, whether IBS, SIBO, other gastrointestinal disorders like Crohn's disease, functional gastrointestinal disorders or digestive system issues. Speak to your healthcare provider who will be able to advise you on any diet to follow.
References
- Mayo Clinic. “Small Intestinal Bacterial Overgrowth (SIBO).” https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168
- Cedars-Sinai Newsroom. “Irritable Bowel Syndrome: Mark Pimentel, MD.” https://www.cedars-sinai.org/newsroom/irritable-bowel-syndrome-mark-pimentel-md
- Quadram Institute. “Fibre, Fermentation, FODMAPs and Flatulence.” https://quadram.ac.uk/blogs/fibre-fermentation-fodmaps-and-flatulence/
- ScienceDirect. “Migrating Motor Complex.” https://www.sciencedirect.com/topics/medicine-and-dentistry/migrating-motor-complex
- Takahashi, T. “Mechanism of Interdigestive Migrating Motor Complex.” Journal of Neurogastroenterology and Motility, vol. 18, 2012, pp. 246–257. https://doi.org/10.5056/jnm.2012.18.3.246
- Windsor Centre for Digestive Health. “What Is FODMAP?” https://windsordigestivehealth.com/what-is-fodmap/
- Johns Hopkins Medicine. “FODMAP Diet: What You Need to Know.” https://www.hopkinsmedicine.org/health/wellness-and-prevention/fodmap-diet-what-you-need-to-know
- Cedars-Sinai Medical Center. “Low Fermentation Diet / SIBO Diet.” https://www.siboinfo.com/uploads/5/4/8/4/5484269/low_fermentation_diet.pdf
- Velasco-Aburto, S., Llama-Palacios, A., Sánchez, M. C., Ciudad, M. J., and Collado, L. “Nutritional Approach to Small Intestinal Bacterial Overgrowth: A Narrative Review.” Nutrients, vol. 17, no. 9, 2025, p. 1410.
- Velasco-Aburto, S., Llama-Palacios, A., Sánchez, M. C., Ciudad, M. J., and Collado, L. “Nutritional Approach to Small Intestinal Bacterial Overgrowth: A Narrative Review.” Nutrients, vol. 17, no. 9, 2025, p. 1410.
- Bek, S., Teo, Y. N., Tan, X.-H., Fan, K. H. R., and Siah, K. T. H. “Association Between Irritable Bowel Syndrome and Micronutrients: A Systematic Review.” Journal of Gastroenterology and Hepatology, vol. 37, 2022, pp. 1485–1497. https://doi.org/10.1111/jgh.15891