Most of us are familiar with vitamin C and how its powerful antioxidant properties can benefit our immune system. But can it also play a role in digestive health?
If you’ve ever taken a high dose of vitamin C, you may have noticed one of its more immediate effects: a sudden urge to find the nearest bathroom.
So what does that mean for IBS sufferers?
For those struggling with irritable bowel syndrome (IBS) - a chronic gastrointestinal disorder that causes pain, cramping, and bouts of diarrhea or constipation— the big question is, does vitamin C help the problem or make it worse?
Since IBS has no single known cause and varies from person to person, it can be difficult to manage. Let’s break down how vitamin C interacts with IBS symptoms—and whether it helps, hurts, or does a little of both.
Key Takeaways
- Irritable bowel syndrome (IBS) is a chronic gut disorder with subtypes like IBS-D, IBS-C, and IBS-M, driven by factors such as altered motility, gut hypersensitivity, dysbiosis, and stress.
- Vitamin C can act as a gentle osmotic laxative that may help relieve constipation in IBS-C by drawing water into the intestines and supporting more complete bowel movements.
- High doses of vitamin C or very acidic forms can worsen IBS-D and some IBS-M cases by triggering diarrhea, gas, or bloating, so dose and form matter.
- Most people with IBS do best starting with buffered vitamin C at 500 to 1,000 mg and carefully titrating up only as tolerated while watching for loose stools.
- For long term IBS relief, building a healthier microbiome with well tolerated prebiotic fibers is more important than chasing short term laxative effects from vitamin C alone.

What Exactly is IBS?

Irritable bowel syndrome (IBS) is a common gastrointestinal disorder affecting around 11% of the global population.(1)
It’s primarily characterized by abdominal pain, bloating, and changes in bowel habits. But symptoms and severity vary widely from person to person. IBS is typically classified into three subtypes based on symptoms:
- IBS-D (Diarrhea-Predominant): Frequent loose stools and urgency.
- IBS-C (Constipation-Predominant):Infrequent bowel movements, often with difficulty passing stool.
-
IBS-M (Mixed Type):Alternating between diarrhea and constipation.
While IBS doesn’t increase mortality risk, it can significantly impact quality of life, leading to discomfort, stress, and frustration over unpredictable symptoms.
Some people with IBS also experience other gastrointestinal conditions. Such as small intestinal bacterial overgrowth (SIBO), leaky gut, or food sensitivities.
Related Post: Best Probiotic for Women
What Causes IBS?

While the exact cause of IBS isn't clear, research suggests it’s a complex biopsychosocial disorder—meaning that a mix of psychological, biological, and environmental factors contribute to its development.(2)
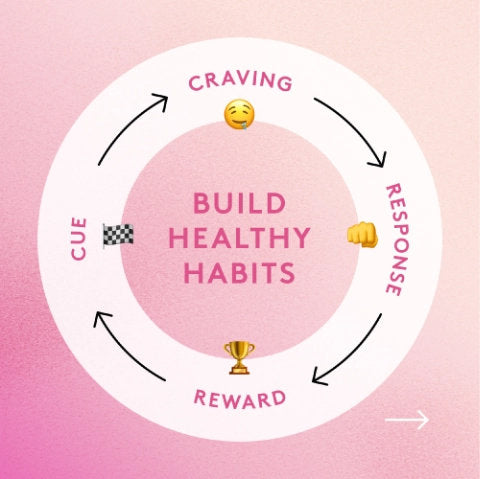
Three key mechanisms appear to drive IBS symptoms:
- Altered Gut Motility: The digestive system contracts too quickly (leading to diarrhea) or too slowly (leading to constipation).
- Heightened Gut Sensitivity: The intestines overreact to normal digestion, causing pain and cramping.
- Gut-Brain Connection: The nervous system and gut interact closely, and stress or anxiety can exacerbate IBS symptoms.
In addition to those, a few other underlying factors can contribute to IBS, including:
- Gut dysbiosis: An imbalance in gut bacteria.
- Small intestine bacterial overgrowth (SIBO):Excess bacteria in the small intestine can worsen bloating and IBS symptoms.
- Leaky gut: Increased intestinal permeability may lead to inflammation.
- Food intolerances: Sensitivities to gluten, dairy, FODMAPs, or artificial sweeteners can trigger symptoms.
How is IBS Treated?
There’s no one-size-fits-all cure for IBS. Medications are available to relieve symptoms of IBS, but if you're looking to ease IBS as naturally as possible, dietary and lifestyle changes are often the most effective.

Dietary Changes For IBS Relief
If you deal with bloating, diarrhea, or abdominal pain, adjusting your diet can make a big difference.
- Caffeine and fatty foods can overstimulate the colon, making IBS-D symptoms worse. Cutting back may help reduce urgency and discomfort.
- Certain carbohydrates are harder to digest and can lead to excess gas and bloating. The main culprits? Lactose, fructose, and sorbitol—common in dairy, fruit, and sugar-free products.
- Trying an elimination diet can help you pinpoint specific food triggers. Common ones include gluten, dairy, and FODMAPs—fermentable carbs that can worsen IBS symptoms.
Medications for IBS (Symptom Management, Not a Cure)
Medications can also be used to treat IBS, although it's rarely recommended as the first line of defense. This is because they tend to tame, not treat. However, for severe cases, doctors may recommend medications such as:
- Smooth muscle relaxants (for cramping).
- Antidiarrheal medications (for IBS-D).
- Laxatives (for IBS-C).
- Low-dose antidepressants (to regulate gut-brain signaling).
Alternative Therapies & Emerging Treatments

There are some alternative methods that may help manage symptoms for IBS sufferers, including:
- Probiotics – While some people benefit from probiotic supplements, the choice of strain matters. Not all probiotics work for IBS, and some may worsen symptoms, depending on individual gut sensitivity.
- Prebiotics – Rather than introducing new bacteria, prebiotics feed and strengthen beneficial gut microbes, helping to improve gut balance. Certain types, like Orafti® Synergy1 (inulin-FOS from chicory root), are well-tolerated and support both digestion and immune function.
- Gut-directed hypnotherapy, psychotherapy & cognitive behavioral therapy (CBT) – These approaches help regulate the gut-brain connection. Not only can this reduce stress-related flare-ups, but there's a strong connection between the nervous system and colonic function.(3)
- Acupuncture & massage therapy – Some people report symptom relief from these therapies, likely due to their ability to support relaxation and reduce gut hypersensitivity.
Now that we’ve covered IBS basics, let’s look at whether vitamin C plays a role in symptom relief—or whether it makes things worse
Learn more about other vitamins for IBS here
Can Vitamin C Help IBS?

We know vitamin C has amazing antioxidant properties and immune benefits. But its effects on IBS symptoms depend largely on the dose, form, and individual response.
For people with IBS-C, insufficient peristalsis can lead to severe discomfort; there isn't enough contractile activity to completely evacuate the bowels (4).
Vitamin C may offer relief by acting as a natural osmotic laxative. It draws water into the intestines, softening the stool and promoting bowel movements—similar to how magnesium citrate works.
In fact, some people with IBS-C use high-dose buffered vitamin C powders (combined with minerals like potassium, calcium, and magnesium) to stimulate peristalsis—the wave-like contractions that push food through the intestines.
While results vary between people, this has produced a powerful but safe laxative effect within 90 minutes.
Effervescent vitamin C powder (4,500 mg of ascorbic acid buffered with magnesium carbonate) has also shown equally effective results, but the dose should be adjusted to the individual; if you're experiencing diarrhea, pull back on the amount.
If you're looking for relief from IBS, over-the-counter medications will relieve symptoms, but they won't solve the problem.
Similarly, vitamin C supplementation has been shown to benefit those that struggle with constipation from IBS-C, but increasing your vitamin C intake won't be the end of IBS.
Does Vitamin C Worsen IBS Symptoms?
While vitamin C can relieve constipation, high doses may trigger diarrhea, which could worsen symptoms for IBS-D sufferers.
- If you struggle with IBS-D (diarrhea-predominant IBS), excessive vitamin C may exacerbate urgency and loose stools.
- Some people also experience bloating and gas if they take acidic forms of vitamin C (like ascorbic acid).
Finding the Right Dose for IBS-C Relief
As mentioned, for those with IBS-C (constipation-predominant IBS), vitamin C’s mild laxative effect can be beneficial. However, dosing should be adjusted gradually to avoid overdoing it.
- Start with 500-1,000 mg of buffered vitamin C per day.
- Increase slowly up to 4,000 mg, if tolerated, to encourage bowel regularity.
- If diarrhea occurs, reduce the dose to find a balance that works for your digestion.
By choosing the right type and amount of vitamin C, you can support your gut health without triggering unwanted side effects. If you’re unsure where to start, opting for a buffered or food-based form is usually the best approach.
If you want to kick IBS to the curb for good though, working on gut health should be a top priority - and something like Performance Lab® Prebiotic can be a solid place to start.
Beyond Vitamin C: Supporting Long-Term Gut Health

While vitamin C can provide short-term relief for IBS-C, managing IBS effectively requires more than just symptom relief. The key to long-term gut health lies in nourishing the microbiome—the community of bacteria in your digestive system that influences digestion, inflammation, and overall well-being.
For many people with IBS, gut bacteria imbalances ( gut dysbiosis) can make symptoms worse. This is where prebiotics come in. Unlike probiotics, which introduce new bacteria, and in some cases, may cause further upset. Prebiotics feed and strengthen the beneficial bacteria already in your gut, helping to restore balance and improve digestion.
Performance Lab® Prebiotic is designed specifically for this purpose. It contains Orafti® Synergy1 (a highly effective inulin-FOS blend from chicory root), which selectively nourishes Bifidobacteria—a gut-friendly bacterial strain linked to improved digestion, reduced bloating, and better stool consistency.
Related Post: Inulin and IBS: What's The Link?

By incorporating a high-quality prebiotic into your routine, you’re not just addressing IBS symptoms—you’re building a stronger, healthier gut that can function more efficiently in the long run.
Shop Performance Lab® Prebiotic
References
- Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71-80.
- Camilleri M. Management of the irritable bowel syndrome. 2001;120(3):652-668.
- Ballou S, Keefer L. Psychological Interventions for Irritable Bowel Syndrome and Inflammatory Bowel Diseases. Clin Transl Gastroenterol. 2017;8(1):e214.
- Grassi M, Petraccia L, Mennuni G, et al. Changes, functional disorders, and diseases in the gastrointestinal tract of elderly. Nutr Hosp. 2011;26(4):659-668.