Key Takeaways
- The carbohydrate insulin model claims that carbs and insulin drive fat gain by pushing calories into fat cells, but this view is overly simple.
- Evidence shows that protein also stimulates insulin, high protein diets can support fat loss, and people can stay lean on high carb diets when energy balance is controlled.
- Different types of carbohydrates have very different effects on hunger, blood sugar, and body weight, so quality matters as much as quantity.
- Overall energy balance, diet quality, activity levels, and sustainable habits are more important for fat loss than focusing on insulin alone.

Introduction to Carbohydrate-Insulin Hypothesis
Recently, diets that are very low in carbohydrates, like the ketogenic or ‘keto’ diet, also known as a very low carbohydrate diet, have become very popular and some people believe they are an effective solution for body weight regulation and combating obesity.
There’s good evidence that these diets can help people lose body fat. However, there’s some debate about how exactly they work.
Traditionally, it was thought that these diets helped people lose weight because they ate fewer calories than they burned (this is known as being in a “negative energy balance”). This calorie reduction was believed to come from eating less carbs.
But there’s another theory called the carbohydrate insulin model (CIM)— also referred to as the Carbohydrate-Insulin Hypothesis — that challenges this old idea. According to CIM, the main reason people gain weight isn’t just about eating too many calories compared to what they burn
Instead, CIM suggests that the real problem is carbs and the insulin hormone that our bodies release when we eat carbs. This model proposes that insulin plays a big role in causing obesity.
Related Posts:
What is the Carbohydrate Insulin Model?

The Carbohydrate Insulin Model is a theory about how our bodies handle carbohydrates and manage body fat.
Here’s how it works:
Carbohydrate Digestion
When you eat foods containing carbohydrates, these are broken down into glucose, which raises your blood sugar levels.
Insulin Production
In response to this increase, your body produces insulin, a hormone that signals cells to take in glucose for storage (as glycogen in liver and muscles) or to use as energy. This insulin secretion helps lower your blood sugar.
Impact on Body Fat
High insulin levels promote fat storage as the body prioritizes dealing with blood glucose over burning body fat for energy. This shift leads to an increase in fat storage which can lead to weight gain.
Changes in Energy Dynamics
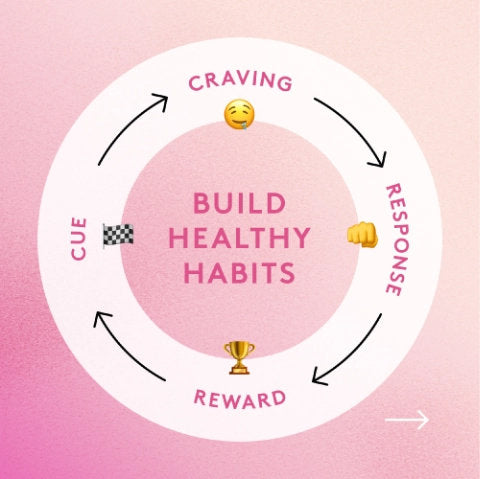
The carbohydrate insulin model suggests that these actions affect overall energy dynamics by increasing total energy intake (how much you eat overall) and reducing energy expenditure (the energy you use). This happens because elevated insulin levels can make you feel hungrier and less inclined to be active, promoting a positive energy balance.
In summary, according to this model, eating carbohydrates leads to changes in blood sugar and insulin levels that may increase fat storage, make you eat more, and decrease the amount of energy you use.
What are the Criticisms of the Carbohydrate Insulin Model?
The Carbohydrate Insulin Model (CIM) has come under fire for its explanations of body weight regulation and body fat management. Here are the top eight:
1: Protein and Insulin Interaction
The CIM fails to account for the fact that protein also triggers significant insulin release. Like carbohydrates, proteins are broken down into amino acids which require insulin to be absorbed into cells. Critics argue that if insulin is problematic for body fat accumulation as CIM suggests, then protein should also be implicated, which it is not in the model.
2: Effects of High-Protein Diets

Contrary to the implications of the CIM, diets high in protein have been consistently beneficial in promoting loss of body fat. This poses a question on the CIM’s focus on insulin’s role in fat storage.
3: Questionable Impact on Energy Expenditure
The CIM’s claim that carbohydrates and insulin significantly lower daily energy expenditure is not widely supported by evidence. The energy balance model (EBM) addresses regulated energy homeostasis but falls short in explaining the rising prevalence of obesity. In fact, some carbohydrate types are known to improve hunger control better than fats, which can positively affect energy balance.
4: Insulin's Potential Benefits on Hunger
There are indications that insulin may actually help decrease hunger levels, which contradicts the model’s assumption that increased insulin from carbohydrate intake worsens obesity.
5: Complex Carbohydrate Effects on Body Weight

Different types of carbohydrates (especially those high in fiber) affect body weight management and hunger differently. These nuanced effects are often overlooked in the CIM, which oversimplifies how carbohydrates influence fat storage and hunger.
6: Observational Data Misinterpretation
The CIM was partly supported by data linking high sugar intake from low fat diets to obesity increases in the past. However, despite reductions in sugar consumption, obesity rates continue to climb, indicating that other factors must influence body fat trends.
7: Real-World Examples in Athletes
Many athletes maintain low levels of body fat even with high carbohydrate intake due to their overall high energy expenditure. This includes endurance athletes and bodybuilders, who often consume substantial carbs yet manage body weight effectively, contradicting the CIM’s assumptions.
8: Fat Metabolism After Meals
Post-meal fat metabolism also disputes the CIM. Adipose tissue plays a crucial role in hormonal responses, metabolic fuel availability, and body weight regulation. Following a high-fat, low- carb meal, fats are stored even with low insulin levels, due to the action of Acylation Stimulating Protein (ASP), which promotes fat storage. This shows how total dietary fat management is more complex than simply insulin levels and challenges the core of the CIM’s argument regarding energy balance.
These points highlight the significant theoretical and practical challenges to the Carbohydrate Insulin Model, questioning its validity in fully explaining the dynamics of energy balance, body weight, and body fat.
Research Supporting the Carbohydrate-Insulin Model

Despite these criticisms, there is a small number of papers that appear to show low carb diets are effective for fat loss. Possibly more so than a ‘straight' calorie deficit. Some key points and studies supporting the carbohydrate insulin model include:
Insulin's Role in Fat Storage
Research has shown that insulin plays a significant role in fat metabolism, specifically in promoting fat storage and inhibiting fat breakdown. This supports the CIM's argument that insulin response from carbohydrate intake may lead to increased fat storage.
Effects of Low-Carbohydrate Diets
Several studies have reported that low-carbohydrate diets can lead to weight loss and improvements in various metabolic markers without the need for caloric restriction. These diets tend to lower insulin levels, which, according to the CIM, would decrease fat storage and increase fat oxidation.
Controlled Feeding Studies
Some controlled feeding studies suggest that diets with a lower glycemic load (which cause less of an insulin spike) can lead to greater energy expenditure and fat loss compared to high-glycemic diets, even when caloric intake is the same.
For example, a study by Ebbeling et al. found that participants on a low carbohydrate diet experienced higher energy expenditure during weight loss maintenance compared to those on high carbohydrate diets.
While limiting your carbs, ensure you up your fiber intake as well with a low carb diet fiber supplement.
Longitudinal Observations
Observational studies have linked high-glycemic diets with greater incidence of obesity and type 2 diabetes, supporting the idea that the quality of carbohydrates can influence insulin dynamics and weight gain.
Despite these supporting points, it is important to note that the CIM is not universally accepted. Some researchers argue that calorie balance remains the most crucial factor in weight loss and that the effects of insulin are a part of a broader set of hormonal and metabolic responses.
Research Challenging the Carbohydrate-Insulin Model

A lot of existing research questions the validity of the Carbohydrate-Insulin Model (CIM). Extensive long-term weight loss studies in both humans and animals, which are meticulously controlled and ensure protein levels are consistent, have demonstrated that fat loss is similar across various dietary compositions. This finding underscores that dietary composition may not be as critical as once thought, provided protein intake is equated.
Why is protein so important?
Because it has a high ‘thermic effect'. Meaning that we actually do have an increase in energy expenditure due to the digestion and absorption of protein. This affects our energy balance. Interestingly, carbohydrates also exhibit a higher thermic effect compared to fats, suggesting a slight theoretical advantage to higher carbohydrate diets, though the practical impact of this is minimal.
Implications for the Calories In, Calories Out Model
This does not refute our CICO model. It just highlights that macronutrient intake subtly affects it, reflecting the dynamic nature of our metabolic processes. If low-carbohydrate diets offer any particular benefit, it likely stems from higher protein intake rather than the ratio of fats to carbohydrates.
This brings us back to the Ebbeling et al. study mentioned above.
Critique of Supporting Studies
The study by Ebbeling et al., adjusted its study outcomes post hoc and altered the timing and duration for assessing total energy expenditure (TEE) across different carbohydrate intake groups. Although TEE was initially higher in the low-carbohydrate group, both before and after the maintenance phase, the overall change in TEE was not significant and appeared to be influenced by pre-intervention differences rather than by the diet itself.
There were a number of participants in the group who had significant amounts of ‘unaccounted energy'.
Some participants had significant discrepancies in their energy accounting, suggesting over 600kcal per day of unexplained energy while remaining weight stable, raising serious doubts about the accuracy of diet control, the method used to assess TEE, and the assumptions underlying these measurements. Such discrepancies challenge the validity of conclusions drawn about the efficacy of low-carbohydrate diets and point to potential flaws in study methodology.
Further Issues with Study Methodologies
In addition to the previously mentioned critiques, specific concerns arise regarding the methods used to assess TEE and the assumptions underlying the calculations. These issues are in direct conflict with the laws of physics and suggest possible inaccuracies in several areas:
-
Diet Control and Compliance: There were indications that some participants may have consumed additional foods not accounted for in the study. This brings the accuracy of the dietary control and macronutrient amounts into question, potentially skewing the results.
-
Methodological Flaws: The method used to assess TEE has been criticized for its validity. If flawed, this would make it inappropriate to suggest that TEE actually differed significantly between the dietary groups.
-
Respiratory Quotient (RQ) Assumptions: The assumptions made to calculate TEE were based on non-measured RQ values. The RQ, which is the ratio of oxygen uptake to carbon dioxide production, indicates the types of fuel the body is using. Even minor inaccuracies in RQ values could lead to no observable differences in TEE across diets, questioning the metabolic impact claimed by the CIM.
-
Unexplained Energy Efficiency: Surprisingly, the data suggested that the low-carbohydrate group maintained weight despite having a higher TEE, which could imply an unexplained increase in metabolic efficiency. This phenomenon contradicts expectations from a thermodynamic perspective and raises further doubts about either the data accuracy or the biological plausibility of the results.
For those of you who wish to dissect these arguments in more detail, then both the original study, and the follow up critique/analysis by Hall et al. are linked at the bottom of this article.
There are also a series of ‘letters to the editor' between these research groups addressing the above points.(1,2,3,4)
Conclusion on the Carbohydrate-Insulin Hypothesis and Model
Although the CIM has some rationale supporting it, many of the assumptions fall down under more detailed scrutiny.
The model proposes that insulin related to carbohydrate intake is a primary driver of obesity, but the evidence supporting this claim remains inconsistent and is often questioned for its scientific robustness.
Fundamentally, the prevailing principle in understanding fat loss remains the energy balance equation, encapsulated by the Calories In, Calories Out (CICO) model. This model acknowledges that while energy balance is influenced by macronutrient composition, it is ultimately the balance of calories consumed versus calories expended that dictates weight management.
To date, there is no compelling evidence to suggest this viewpoint should be changed. Research supporting the CIM often originates from a single research group, which could potentially introduce bias.
In conclusion, while it is essential to continue exploring various perspectives in obesity research, claims made by the CIM should be approached with caution until more robust, replicated studies are available.
References
-
Ludwig DS, Ebbeling CB. The Carbohydrate-Insulin Model of Obesity: Beyond "Calories In, Calories Out". JAMA Intern Med. 2018 Aug 1;178(8):1098-1103. doi: 10.1001/jamainternmed.2018.2933. PMID: 29971406; PMCID: PMC6082688.
-
Ebbeling CB, Feldman HA, Klein GL, Wong JMW, Bielak L, Steltz SK, Luoto PK, Wolfe RR, Wong WW, Ludwig DS. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial. BMJ. 2018 Nov 14;363:k4583. doi: 10.1136/bmj.k4583. Erratum in: BMJ. 2020 Nov 3;371:m4264. PMID: 30429127; PMCID: PMC6233655.
-
Hall, K.D., Guo, J. & Speakman, J.R. Do low-carbohydrate diets increase energy expenditure?. Int J Obes 43, 2350–2354 (2019). https://doi.org/10.1038/s41366-019-0456-3
-
Hu S, Wang L, Togo J, Yang D, Xu Y, Wu Y, Douglas A, Speakman JR. The carbohydrate-insulin model does not explain the impact of varying dietary macronutrients on the body weight and adiposity of mice. Mol Metab. 2020 Feb;32:27-43. doi: 10.1016/j.molmet.2019.11.010. Epub 2019 Nov 16. PMID: 32029228; PMCID: PMC6938849.